
Linda Nguyen has dedicated half a decade working at Ambulance Victoria as a Triage Practitioner after leaving behind the world of hospital emergency care
After eight years working in an emergency department, Linda said she needed a change of scenery that kept her passion alive for frontline emergency health care.
“I wanted to still be able to utilise my skills as an emergency nurse whilst maintaining some form of patient contact. I enjoy working with my patients, building a positive relationship with my community that in turn creates a better understanding between the healthcare system and the needs of my patients,” she said.
As a Triage Practitioner, Linda’s role sees her conducting the initial assessment of patients who have requested assistance by calling Triple Zero (000). From there, she determines the most appropriate and best care for their condition.
“As part of the service, I can provide alternative services other than an ambulance – this may include a locum or a nurse to visit who can treat the patient in the home, a telehealth assessment, or a mental health clinician. There are many services in the community that we can offer patients.”
As a Triage Practitioner, Linda says it’s often difficult to predict what may happen at any time during a patient assessment. In some cases, assessments and conversations with patients may be lengthy, while other cases Linda and her team may work with patients who are quite unwell and require an ambulance dispatch.
“The most rewarding part of my job is being able to connect with my patients and help them the best way I can. What most people don’t realise is that despite being behind a phone, there is so much rapport I can build with the patient. COVID impacted my personal life just as much as my patients. I can empathise with a parent who is calling about concerns for her child who is sick, or even a family who has concerns for their elderly grandparent. I am a parent myself and I have family who I care about – as a health care professional, I have been able to experience both sides of being the patient and the provider. This is what drives me to do what is best for my patients – knowing that when I put myself in their shoes, I want my health specialist to advocate what is best for me,”, she said.
Ambulance Victoria’s Triage Services has a team of trained paramedics and nurses who can conduct a comprehensive triage assessment over the phone.
“The very reason for our existence is that not everyone calling 000 may need an ambulance, and so we cater for that. There are so many services that we can offer patients which are more suitable to their needs rather than requiring an ambulance and being transported to hospital.”
Linda’s best piece of advice to anyone considering working in Triage Services?
“Here within Triage Services, we are a team of compassionate healthcare professionals, and we advocate for best patient care. The environment is challenging yet rewarding and there are many opportunities for career progression and growth with us. We welcome anyone who holds the required skillset and passion to make a difference within our community.”

For Waseem, the month of Ramadan is a time for spiritual reflection. A time when Waseem and his family reflect on what is important in life and on what they feel most thankful for.
“It is also a time to reflect on your own actions and how you can improve yourself to be the best person you can be to your family, friends, colleagues, and the wider community.”, says Waseem.
“It is also a time to reconnect and reset with your faith as Ramadan is a month of charity, helping others who are less fortunate than yourself and it is also the month that most Muslim’s use to pay their Zakat (mandatory pillar of Islam where you pay a portion of your wealth to charitable causes annually).”
Fasting during the month of Ramadan usually occurs from pre-sunrise to sunset, every day.
“Fasting teaches you to be patient, (to) control your emotions/feelings, and to be thankful for what you have. It’s not just abstaining from eating and drinking from dawn to dusk but it is also (about) teaching you to control your temper and emotions whilst fasting.
For me personally, it teaches me to be thankful that I am fortunate enough to be able to provide food, clothing, and shelter for my family – a basic right many people around the world do not have.”
For those wanting to know more about the holiday, Waseem encourages those who identify as non-Muslim to go ahead and ask questions.
“Please don’t feel like you can’t eat around us, or (that) you’ll tempt us to break our fast. Fasting is a mental and spiritual exercise as much as it is a physical one. We are doing it for our Lord and ourselves. Feel free to ask questions, there are no stupid questions (Yes, we cannot eat OR drink… yes that includes water).”, says Waseem
Going without his morning coffee for the first few days of Ramadan is the biggest challenge for Waseem.
“Especially if I’m on shift! Other than that, I guess it does take a couple of days to get your body used to fasting, however I believe it is also a mindset thing as well.”
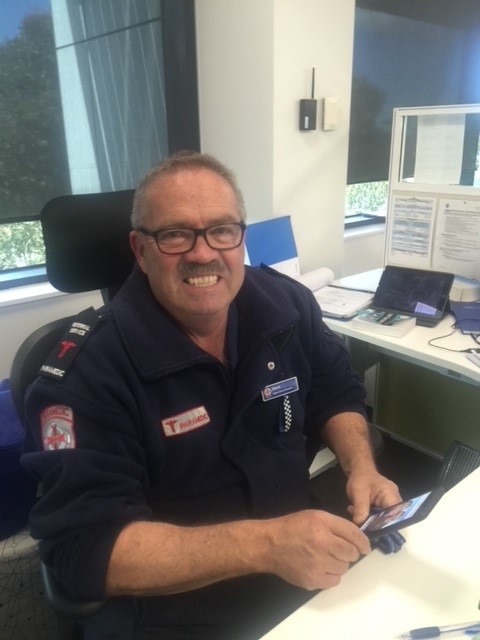
It was 1982 when Stephen Bird started his career as a paramedic with Ambulance Victoria.
Fast forward to this Tuesday, 12th April and the well-respected colleague will have clocked up 40 years since that first day on the job.
A testament to his character and determination, Stephen says he has the same enthusiasm and passion for helping people in their time of need as he did on his first day.
The country boy from Neuarpurr credited the resilience that comes from growing up on a farm to enabling him to make the switch from nursing to being a rural paramedic in Horsham and then onto bustling Melbourne.
“Back then it was unheard of for paramedics in the country to come to the city,” he said.
“I was a bit of a lost young bloke. I just wanted to go where the work was.”
“I wanted to be somewhere where I could learn new skills and I just loved the excitement of being a young paramedic in Melbourne.”
Over the past four decades, Stephen has witnessed the organisation grow into the state-wide service we know it as today; first on the road as a paramedic and then as the first paramedic to join the organisation’s communications centre in 1988. To this day, he still provides clinical advice by phone through Ambulance Victoria’s Secondary Triage service as a Referral Service Triage Practioner (Paramedic).
“When the new communications centre opened it was like the changing of the guard,” Stephen said.
“I was one of the first paramedics to complete the new communications course when we went to the Doncaster communications centre. It was staffed by experienced paramedics who were also communications officers.”
“I’m a big fan of anyone in ambulance wanting to do better. I took every opportunity that came my way.”
When asked to describe Ambulance Victoria during his time in the service, Stephen said he found the organisation had evolved to be “diverse, professional and empowering”.
“It’s hard to name a highlight because there’s been so many. I was 27 when I joined,” he said.
“But the highlight is when you deliver your first baby. Some paramedics may not deliver any, but I’ve been fortunate to deliver 8 babies all up. That never gets old.”
“There’s also saving someone, caring for someone who is palliative…It’s not always shootings and accidents.”
Although Stephen has been involved in his fair share of those over the journey, too. From both the Queen Street Hoddle Street massacres, to the Russell Street bombing and Mercy Hospital shooting, Stephen has found himself responding to some of the biggest events Victoria has experienced.
“I might have left the road a long time ago, but I feel very proud to be a paramedic. There’s not really another job like it,” he said.
“I was so excited when I started in ambulance. I still believe we have the best ambulance service in the world.”

Sarah’s 18 years with Ambulance Victoria (AV) have entailed a number of adventures and breathtaking highs and lows – none quite so literal as becoming one of AV’s first female MICA flight paramedics.
Sarah’s passion for paramedicine was ignited when completing a first aid course delivered by paramedics in her VCE years.
“This was the first time I had thought of a job I would actually like to do.”
Nearly two decades on, Sarah’s time as a paramedic has seen her attend to patients all across Victoria. This includes one of her first cases at air ambulance when she landed on a small island in Western Port Bay.
Sarah says the most rewarding aspect of her role is the connections she makes with people on these adventures. This includes patients, their families, emergency services, hospital staff and, of course, her colleagues.
She is currently working a short stint on road after having a baby but will soon return to her role as a MICA flight paramedic.
“I am so fortunate to have had this time off and I am deeply grateful to my colleagues who worked tirelessly throughout the last two years.”
When Sarah does return to the skies, she will be supported by air crews including specially trained pilots who spend years dedicated to preparing for the role.
“People always ask if we fly the helicopter as well. I can barely get myself in and out of the seatbelts, there is no way I would be able to or want to fly it.”
Sarah’s best piece of advice to anyone considering becoming a MICA flight paramedic?
“Don’t do it for the helicopter rides – do it for the lessons, the skills, the training, the experience and the humility.”

Over two years ago, Amanda was on her way to go kayaking with a friend, an off-duty paramedic, when her GoodSam app alerted her to a life-threatening emergency close by.
It turned out to be a life-changing event – not just for the patient but for Amanda, too.
“Our actions on arrival probably stopped the patient from going into cardiac arrest,” says Amanda.
“To be fair I just did as I was instructed, so all the credit goes to my friend.
The ambulance that later arrived happened to have an Ambulance Community Officer (ACO) working alongside a paramedic, and I thought – that’s awesome, I want to do that job!”
An ACO role with Ambulance Victoria combined three of the most important things Amanda was looking for in a career – excitement, responsibilities which challenged her, and a way to help people in need. Amanda’s now been with AV for two years.
“I love being able to provide help and reassurance to someone who may be going through some of the hardest moments of their life.”
Neither pre-existing medical knowledge nor skills are compulsory to apply to become an ACO as Ambulance Victoria provides all the training required.
“We have people from all ages and backgrounds, including plumbers and bank managers, who become Ambulance Community Officers to help their local community.”
Amanda’s role as an ACO has furthered her passion for delivering emergency healthcare to those in need and has now prompted her to start studying her paramedicine degree.
While being an ACO has its normal challenges, the COVID-19 pandemic has brought all new ones, particularly during its peak in Victoria. Whilst her attitude has remained positive, these challenges have called for Amanda to take on a new scope of responsibility.
This includes being part of Ambulance Patient Offload Teams which help care for patients arriving at hospital emergency departments and allow ambulances to get back into the community for emergencies.
“The role has increased since the start of the pandemic, but it is very rewarding, and I learn something new with every shift.”

Ken Whittle, a Peer Responder with AV’s Wellbeing and Support Services, has been working with the organisation for 24 years- but not always as a Peer Responder and not always with his trusty sidekick, Bruce.
“I did a few different things before joining the Metropolitan Ambulance Service (as it was known back then). I think my interest sparked from “Emergency”, a US TV show in the mid 70’s based on the working lives of two paramedic fire fighters in Los Angeles.”
Over his career with AV, Ken has encountered great “sadness and tragedy“, particularly around the more challenging cases he’s attended as a paramedic.
“I think it is something only those at the scene will truly understand. Things like the death of a child is so very traumatising for the family, some of that sometimes rubs off on to paramedics and other emergency services workers.”
The highlights of Ken’s long-standing career span from delivering babies, to achieving great outcomes when patients’ conditions initially seemed grim, to working in the Peer Support Dog Program with his trusty four-legged sidekick, Bruce.
“Working in the Peer Support Dog Program with Bruce was right up there. It was so special seeing so many AV employees from first day Grads to 30-plus years’ service paramedics. From new administrative staff to senior execs and paramedics and administrative staff alike, (all) smile when Bruce is in the room. No one said they felt worse when patting Bruce. FYI, Bruce loves it also. He gets very excited when he sees the Peer Dog jacket come and he knows he going visiting.”
How did Ken and Bruce’s stories collide? AV’s Wellbeing and Support Services asked for expressions of interest from existing Peers to nominate for a Trial of a Peer Dog program. Both Peers and their dogs were assessed for their suitability as a team. Bruce was a star, as were numerous other dogs owned by other AV Peers.
“There is really no denying that the room lights up when Bruce is in the vicinity. He has certainly raised the profile of AV’s Peer Support Program and increased awareness and hopefully reduced stigma around mental health in AV employees.”
Peer Support is for all AV staff and first responders not just operational paramedics. The community might also be interested to know that the team have received numerous enquiries from emergency services both in Australia and internationally regarding the AV Peer Support Dog program.
“Peer Support is a great role within AV. Like any job it comes with its own challenges. Nonetheless, it can be very rewarding. You need to have a genuine desire to be of assistance to your colleagues.”

Samuel and Sarah, two of AV’s newest graduate ambulance paramedics are hitting the road for the first time after retiring from their former careers as nurses in the emergency departments of busy Melbourne hospitals.
For Sarah, curiosity took over after she’d spent years watching paramedics walk through the emergency department doors of the hospital.
Driven by the desire to continue to help people when they’re at their lowest, Sarah is fascinated by the level of trust patients place in paramedics, and in what their journey looks like before they reach the emergency department.
“When we’re telling our grandchildren and great grandchildren about this (time), we can say ‘I was a part of that, I was a frontline worker in the hospital and on road, and we helped make the change’,” said Sarah.
Samuel on the other hand, from a young age, has “always wanted to be a paramedic”.
When he was 17, Samuel’s mum was injured in an accident. Paramedics were quick to arrive and are for her. It’s their life-saving efforts that inspired Samuel to go into the line of work.
“People always say there’s a calmness when you see paramedics, so I wanted to be that for someone else,” Samuel said.
While the two recruits are not new to a career in healthcare, being a paramedic presents a world of different experiences and situations. Even despite the changes COVID-19 has brought to paramedic work, Samuel and Sarah are itching to get started.

Josh Ovens has been with Ambulance Victoria (AV) for a bit over a year now since the Simpson Community Emergency Response Team (CERT) was established.
The Simpson CERT is relatively new, having only begun training in July 2020 and becoming officially operational in the first week of October 2020.
Josh said he always had huge respect for AV but never imagined he would “actually have the opportunity to work for them”.
Being a member of the CFA, Josh had seen the incredible work that AV does firsthand, which is the primary reason that led him to apply to become a CERT first responder. When Josh learned that Simpson was getting its own CERT, Josh saw it as an opportunity to further serve the community.
“For me, one of the most challenging aspects of the role is being prepared for anything. I never really know exactly what the situation is going to be once I arrive on scene and being able to adapt quickly to what I’m presented with can be a challenge,” Josh said.
Josh said one of the most rewarding aspects of the role was making a substantial, hands-on difference in someone’s life. Quite often, Josh gets called to people having one of the worst moments of their life.
“To be able to guide them through with excellent medical care, compassion, and empathy is incredibly rewarding,” he said.
Another rewarding aspect for Josh is the amazing relationships formed with the people he work alongside.
“They became family very quickly and I cherish each and every one of them,” he said.
Being a new team, the Simpson CERT has never worked in non-pandemic conditions.
“Something the community might not know about being a CERT is that we are volunteers. We are regular people just giving up a bit of time to help. Personally, I wasn’t aware AV had operational volunteer roles before joining.”
The best piece of advice Josh has for people considering becoming a volunteer is to simply not overthink it.
“All this role requires is a kind heart, a willingness to learn, and a passion to want to help the people in your local community,” he said.

David has recently celebrated 15 years of on-road service in the Clinical Transport Services (CTS) division with Ambulance Victoria.
As a Clinic Transport Officer, David predominately attends to low acuity patients, patients who require a walker or walking aid, and patients who need help to travel to pre-booked medical appointments.
“It’s a unique on-road ambulance role where you work on your own.”
Exceptional patient care remains the focus of CTS but the division faces distinct challenges to that of emergency patient transport services. While David is mindful to give each patient as much time as they require, for instance, he knows it important to accommodate their needs within a timeframe that ensures other patients can access transportation and care.
“Our workload can unexpectedly increase, and so can the distance we travel. It’s all part of our day. (With the support of) our control room, we endeavour to make it work out.”
David’s favourite part of his role is something many wouldn’t experience in the emergency patient transport services division.
“You get to know most of your patients as we see them quite regularly. I have met some interesting people over the years, and they all have a story to share, so a sense of trust exists as they not only discuss their health but also everyday life, too.”
“Oh, and the complimentary offering of sweets at Peter Mac Melbourne is always rewarding!”
Having always had an interest in working in public service, David was strongly encouraged to apply for the role by two of his former colleagues.
“I’m still thankful to the both of them.”
David’s best piece of advice to anyone considering applying for a CTS role?
“If you have the experience, a good work ethic, friendly attitude, exceptional time management, and enjoy driving – welcome.”

It was 1971 when Graeme, a fourth-generation beef farmer from Eildon, decided to volunteer for the Alexandra District Ambulance Service (ADAS).
“In those days it was all people in other careers doing volunteer work, we never got paid or anything. But having worked by myself, the opportunity to be part of a team was a change that I enjoyed,” Graeme said.
“The ADAS was a group of people who came together in the late 1940s because there really wasn’t a service like it for the community. They got a bit of training from the local doctors, and it continued from there.”
Five decades of service later, Graeme has certainly been pivotal in continuing to champion the community’s legacy in pre-hospital care.
“I suppose you don’t think that far ahead when you start out, but I never thought I’d quit, and I don’t have any plans to. I never gave it any thought at all, I just kept doing what I’m doing,” Graeme said about his 50-year milestone.
ACOs operating at a community branch work in pairs and are responsible for providing first response emergency care in response to a Triple Zero (000) call. They may be ‘backed up’ by the arrival of a Paramedic crew but may also be required to treat and transport the patient to hospital.
Graeme said a highlight of his career was having a front row seat to the service as it evolved, with the Metropolitan Ambulance Service, Rural Ambulance Service and ADAS merging in 2008 to become the state-wide Ambulance Victoria service of today.
Graeme has seen many changes in the local ambulance service’s equipment, medications, protocols, and vehicles.
“There’s a local family and I remember carting a baby boy home in a humidity crib. He’s an adult now. I’ve carted three generations of people around with assistance when it was needed,” Graeme said.
As the service evolved, so to have the jobs that Graeme has responded to. He recalls everything from rescuing a group of scouts from the top of Mount Cathedral after they were struck by lightning, to using a water ambulance to assist in boating accidents on Eildon Lake.
“There’s always something different or new to learn,” Graeme said.
Ambulance Victoria Acting Senior Team Manager Murrindindi Phil Irving said Graeme was a “stalwart in the Eildon community” and while many ACOs had served their community for a long period of time, no-one had come close to Graeme’s 50 year achievement.
“When I first came to Alexandra from metropolitan, Graeme had already been an ACO for decades,” he said.
“He was always there offering to cover shortfalls and do what he can to keep the Eildon team going.”
“Thinking of all the jobs he would have gone to over the decades, it would be almost impossible to calculate the amount of coverage and service that the community would have received from Graeme looking after Eildon, Marysville and surrounds.”
Graeme said he loved seeing younger people come into the service because “they take it up with such enthusiasm”.
“It’s a great thing to become involved within your local area. A lot of people find it difficult to meet the time and meet the clinical demands of it all, but I’ll tell you now, it’s one of the most rewarding things I’ve ever done.”
“Being able to provide comfort to people in their most dire moments is something that you never forget.”
This is what it means to put on an ambulance uniform.
Meet Sema Caliskan, one of our newest graduate paramedics. Since the age of 15, Sema wanted to be a paramedic. Her younger brother was her inspiration, after he became very sick as a child and was in and out of hospital. Now at 27, she pulls on the Ambulance Victoria uniform.
“I wanted to give back to the community and the healthcare system for doing everything they could to help him out. This is my proudest moment.”
This year has been extremely emotionally taxing on Sema and her family, after her father was diagnosed with glioblastoma in April.
“From the very night I was given the news, I have prayed that my dad will get to see me in my AV uniform.”
Sema’s prayers have been answered.
Congratulations Sema.

After noticing several Hard of Hearing (HoH) patients were finding it difficult to lip read and interact with staff wearing PPE, Jenna started the initiative AV Healthy Signs. Healthy Signs encourages employees to learn Auslan, sign language used predominantly across Australia, greatly improving interactions between paramedics and patients.
During COVID-19, HoH patients have been at risk of misunderstanding paramedic’s communications, and at a greater risk of experiencing stress, worry, and anxiety due to not always being able to understand what is going on or what is being said. The use of masks, although a source of protection for both patients and paramedics, creates a barrier to effective communication.
AV Healthy Signs is a collaboration between AV and an external Auslan organisation. “There’s been a fantastic uptake” according to Jenna, who says staff can login and watch pre-recorded videos of sign language lessons at any time of the day or night- a great thing for those working nightshift.
Jenna’s thoughtfulness and dedication behind the initiative is just one of the reasons we love having her as one of Our People.
