Early defibrillation in cardiac arrest saves lives
Each year, around 25,000 people in Australia and New Zealand die from cardiac arrests that happen outside of hospital. Less than 1 in 10 patients make it to hospital and survive.
If a GoodSAM responder or a bystander uses a defibrillator, it can cut the time to the first shock by half. This can help double or triple the chances of survival.
But only about 2% of GoodSAM responders actually use a defibrillator in these cases. Finding better methods to help people respond faster and use a defibrillator is a research priority.
What is the FIRST trial?
The FIRST trial is a research project run by Ambulance Victoria and St John New Zealand. The aim is to help GoodSAM responders use defibrillator more often when assisting patients.
The trial in Victoria and New Zealand provided GoodSAM responders with a CellAED®. This device is a small portable defibrillator. The trial will determine if this device can help more people survive 30 days after a cardiac arrest outside of hospital.
The trial will prove if using a small portable defibrillator is practical for emergencies. It will also determine if this can be a method for the public to provide help sooner when someone's heart stops. This study is registered with the Australian and New Zealand Clinical Trials Registry (ACTRN12622000448741). Learn more about the trial and the study protocol.
Why is the FIRST trial important?
The best chance to save someone after a cardiac arrest is in the first few minutes. Performing cardiopulmonary resuscitation (CPR) and using a defibrillator can increase a patient's chance of survival and recovery.
One issue is that defibrillators are often difficult to locate. Most defibrillators are often placed in public areas such as shopping centres. These defibrillators are seldom used after business hours. Yet, 75% of cardiac arrests happen at home. That means people at home usually don’t get help from a defibrillator in time. Less than 1% of out of hospital cardiac arrests are receiving bystander-initiated defibrillation.
GoodSAM responders can help improve rates of bystander CPR and defibrillation. When they assist, patients are more likely to get CPR, be in a shockable rhythm, and get a shock from a defibrillator. But even then, only 16% of them use a defibrillator. This is because public defibrillators are not always accessible, especially in emergencies.
The FIRST trial is trying to make improvements to this. It gives GoodSAM responders their own small defibrillators, so they don’t have to find one nearby. This could make a big difference in saving lives, especially in areas where it’s harder to get help. If it works, this device could be used in more places to make things fairer and help more people survive.
What does the FIRST trial involve?
The FIRST trial included active GoodSAM responders from Victoria and New Zealand. These responders must accept at least one alert every two years. They’re split into two groups. One group will be equipped with the CellAED® portable defibrillator. The other group will use the closest public defibrillator when they respond to a GoodSAM alert.
What is a CellAED®?
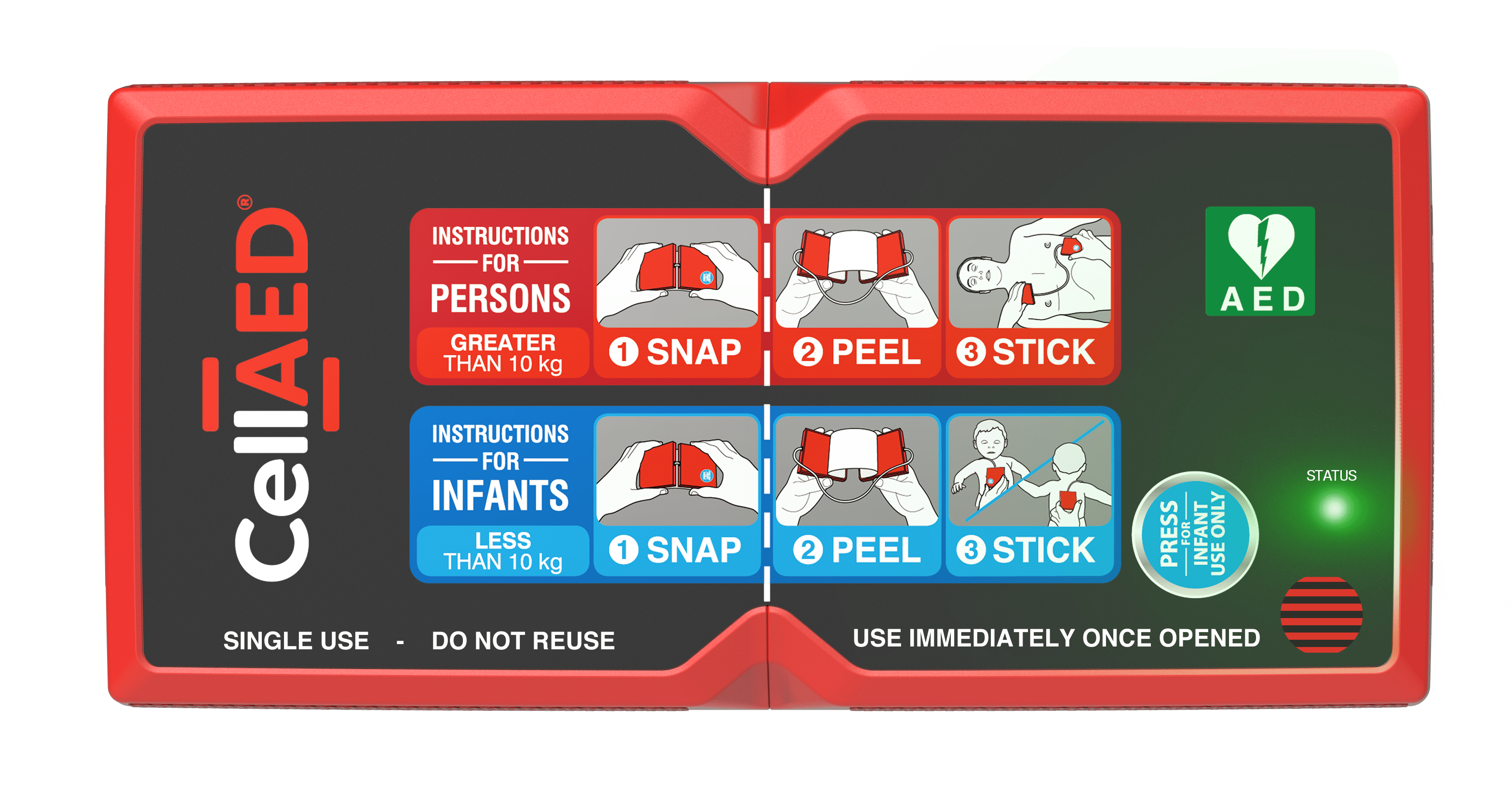
The CellAED® is a small, easy-to-use defibrillator that fits in the pocket and can be used in seconds. It’s fully automatic and for one-time use only. The device has received regulatory approval from the Therapeutic Goods Administration in 2021.
FIRST Resources
Australian and New Zealand Clinical Trial Registration
FIRST Clinical Trial - Training video for GOODSAM participants
FIRST Clinical Trial - Protocol paper
Contact
Ambulance Victoria
Tel: +61418962824
Email: FIRST@ambulance vic.gov.au
St John New Zealand
Tel: +64272070182
Email: FIRST@stjohn.org.nz
Updated
