- Date:
- 30 Oct 2025
Acknowledgement of Country
Ambulance Victoria acknowledges the Traditional Owners of the lands in Victoria. We pay our respects to Aboriginal and Torres Strait Islander cultures and to Elders past and present, and recognise Aboriginal self-determination is a human right.
At Ambulance Victoria, we recognise the diverse and unique cultures and histories of Aboriginal and Torres Strait Islander peoples and value the knowledge of countless generations of Custodians. We commit to working together to build a fair and just future.
We will come together with Aboriginal and Torres Strait Islander communities to identify, understand, and develop opportunities to create and sustain a culturally aware organisation.
Board Chair and CEO report
We are incredibly proud to have the trust of our community as we continued to deliver best care in 2024-25, providing out-of-hospital, mobile and emergency healthcare to more than six million people across more than 227,000 square kilometres.
We are deeply grateful and acknowledge that each improvement and milestone this year has only been made possible thanks to the efforts of our passionate, dedicated and experienced people working and volunteering across every Ambulance Victoria (AV) branch and office across the state.
The year has been marked by great achievements alongside significant challenges, and we are proud of the continued commitment, professionalism and care of our people who remained focused on serving the community while we addressed a number of significant issues impacting the broader organisation.
These included the protracted and challenging negotiation of a new enterprise agreement for our operational staff, the final review into workplace culture by the Victorian Equal Opportunity and Human Rights Commission (the Commission), and growing demand for our services alongside increasing pressure and complexities in the health system more broadly.
We have also engaged with a Parliamentary Inquiry into Ambulance Victoria, led by the Upper House Legal and Social Issues Committee whose review of our service will continue into the coming reporting year.
Despite the challenges encountered, finalising the Ambulance Victoria Enterprise Agreement 2024 (AVEA 2024) marked a key milestone for AV and signalled a commitment to a more collaborative working relationship with our operational workforce and their industrial representatives. The AVEA 2024 is key to creating a more fair, safe and inclusive workplace for our people.
We are working on creating better experiences at work for all our people and rebuilding relationships and trust that may have been impacted during this period. Several improvements to terms and conditions of employment are contained in the AVEA 2024 to ensure AV is a great place to work and volunteer.
Earlier this year, we reached the third and final stage of the Commission’s review into workplace equality in AV, with the final progress evaluation. This provided an initial assessment of our cultural reform progress to date and provided some important feedback to guide our continued focus on building a respectful and safe workplace for the long term.
Sustained culture change takes time, and AV remains strongly committed to our continued improvement across the organisation, by focusing on the issues that are most important to our people. This is reflected in our new People Plan and our continued efforts to build a safe and fair workplace through our daily operations and the way we work.
The Parliamentary Inquiry represents an important opportunity for us to hear from our organisation, our patients and our community about where AV could be doing better still. We engaged (and continue to do so), with a desire to continually improve our workplace for our people and the services we provide for our patients. We look forward to receiving the final report in the coming year.
Over the past year, we’ve made meaningful progress across all four pillars of our Strategic Plan 2023-28 as we strive to become a world leading ambulance service in terms of our people’s experience, patient health outcomes, the impact we make and our connection to each other, our partners, and the broader healthcare system. From deepening community engagement to enhancing operational excellence, we’ve taken deliberate steps to turn strategy into action.
Across 2024-25, our paramedics, first responders, clinicians, volunteers, and corporate teams embraced transformation while consistently delivering and maintaining world-class patient care.
They have done so at a time when the pressure to deliver has not subsided.
The demand for our service continues to grow, seeing us respond to 1,028,393 incidents across Victoria by road and in the air, while our Triage Services team managed 897,771 phone calls.
Our performance data tells the story of dedication under pressure and continuous improvement in the face of record demand.
What has become increasingly clear is that we cannot operate the same way we did 20 years ago, or even five years ago, and expect a different result. New ideas and evidence-based solutions are being developed and rigorously tested, enabling us to continue doing what we do best – serve our communities with dedication, purpose and compassion, even during times marked by uncertainty and ongoing challenges.
Alongside our performance, we are most proud to have delivered Australia’s best cardiac arrest survival rate and the third best in the world following a record year where our connection to and work alongside communities has made a life-changing and genuine impact. This is evidenced by the 2023-24 Victorian Ambulance Cardiac Arrest Registry (VACAR) Annual Report.
Delivering safe and accessible care for as many people as possible was a priority for us in 2024-25. We partnered with the Australian Disability Network and Amaze to develop a fit-for-purpose Neuroinclusion Toolkit to deepen our understanding, support respectful conversations and take meaningful actions that build a neuroinclusive AV for our people and patients.
The toolkit, alongside our Best Care for People with Communication Disability Project with Scope Australia, has been delivered to over 5,500 paramedics to help make healthcare more accessible for everyone.
Our people were supported to continuously learn and grow with programs such as our Paramedic Practitioner program, which has seen two cohorts of students commence their studies.
Currently 28 students are completing their second year of the program, and a further 26 commenced studies in 2025.
This Australian-first program enables paramedics to prescribe and administer scheduled medicines while treating patients on-site, reducing hospital transport needs.
Video Assisted Triage (VAT), our Australasian-first initiative, was expanded across all workstations in our Secondary Triage teams, helping to ensure that 35,092 cases were successfully diverted to appropriate pathways such as the Victorian Virtual Emergency Department (VVED). This ensured more Victorians received the most appropriate care from our expert nurses and paramedics.
The ongoing rollout of our Digital Transformation Upgrade Project (DRUP) continues to have a real impact on our response and readiness. DRUP demonstrated measurable progress with 2,454 staff completing digital radio training, 1,291 portable radios deployed, and 344 vehicles upgraded – a tangible investment in our operational capability that directly supports the delivery of patient care.
And our successful Victorian Ambulance Clinical Information System (VACIS) Modernisation Project delivered more than 5,000 personal issue iPads to paramedics across the state, significantly modernising paramedic patient documentation and equipping our paramedics with the tools they need for efficient care delivery.
As we close the chapter on 2024-25 and look ahead to a new year, we take a moment to pause and reflect. We are proud of what we have achieved together and know our collective efforts have made a real difference worth celebrating. Despite real challenges, our response continues through innovation, collaboration, and unwavering commitment to supporting our people and the Victorian community.
A special thank you to Shelly Park, who concluded her tenure as Board Chair of AV on 30 June 2025. Shelly has shown immense dedication to our people, our service and the Victorian community throughout her time on the Board, and we acknowledge her significant contribution and commitment.
As always and most significantly, we thank our people for their dedication and passion for their work, and for everything they have delivered this year to the people of Victoria.
Jordan Emery ASM, Chief Executive Officer
Andrew Crisp AM APM, Board Chair
Our values
Care
We care in ways that nurture trust and collaboration
- I empathise with our people, patients and community
- I consider how others are impacted by my actions
- I acknowledge good work when I see it
Accountability
We are accountable in our roles and to each other
- I perform my role responsibly, fairly and transparently
- I follow through on the commitments I make and the expectations of me
- I take responsibility for creating a safe environment in which to speak up
Respect
We are respectful and consciously inclusive
- I communicate and act respectfully all the time
- I recognise others’ contributions, unique perspectives and experiences
- I behave with integrity and contribute to a safe workplace
Excellence
We strive to be our best for our people, patients, and communities
- I seek opportunities to continuously develop and grow
- I promote a curious learning environment by teaching, coaching and guiding others
- I collaborate to empower the people around me to deliver quality and be their best
Strategic plan
Belief and purpose
Our belief
We believe that everyone has the right to access quality and effective patient-centred healthcare so that they can live their best lives.
Our purpose
To bring world-leading, patient-focused, out-of-hospital, mobile, and emergency health care to the Victorian community.
Strategic plan
The Ambulance Victoria Strategic Plan 2023-2028: Transforming for better outlines our roadmap for delivering world-leading, patient-focused, out-of-hospital, mobile, and emergency health care to the Victorian community. We are in year two of this comprehensive strategy, structured around four pillars – People, Patients, Impact, and Connection.
In the second year of this plan, we have delivered outcomes in all four of the strategic pillars.
Strategic Pillars
People
In our People pillar, we aim to ensure that our people are engaged, highly trained, equipped and connected, and for our leaders to ensure our people feel valued, safe, healthy and included.
This year a key focus was employee engagement. In 2024-25, we enabled the development of local Employee Engagement Forums across all Ambulance Service Areas in Regional Operations, and we implemented Town Hall events for all divisions.
We recognise that long-term culture change takes time and our journey towards building our safe and respectful workplace continues, with one of the key focus areas for the year ahead being the commencement of delivering the AV People Plan.
Informed by staff feedback and the Victorian Equal Opportunity and Human Rights Commission review, the People Plan was approved in June 2025 and brings together key initiatives including roster reform, diversity and inclusion, health and safety. The plan ensures that our ongoing reform progress is people-centred, sustainable and embedded in our core business.
To support the uplift of leadership capability, this year we continued to deliver the Leading Together Program, with over 500 leaders completing the program so far. The program promotes people-centred leaders who demonstrate compassion, courage and connection as part of their daily leadership practice.
An Anti-Bullying eLearn and Anti-Harassment eLearn launched for all employees, and the Equal Employment Opportunity (EEO) for leaders eLearn was released to all substantive and acting AV leaders.
The Ambulance Victoria Enterprise Agreement 2024 (AVEA 2024) commenced operation in February 2025 following approval by the Fair Work Commission with increased and improved employee entitlements to be delivered over the life of the four-year agreement.
Negotiations are underway for the Ambulance Victoria (Management and Administrative Staff) Enterprise Agreement 2025 (AVMA 2025), helping to ensure improved working conditions for all of our people.
Patients
The Patients pillar aims to provide patients across Victoria with world leading mobile and emergency care that is timely, culturally sensitive and connected, with optimal clinical outcomes and patient experience.
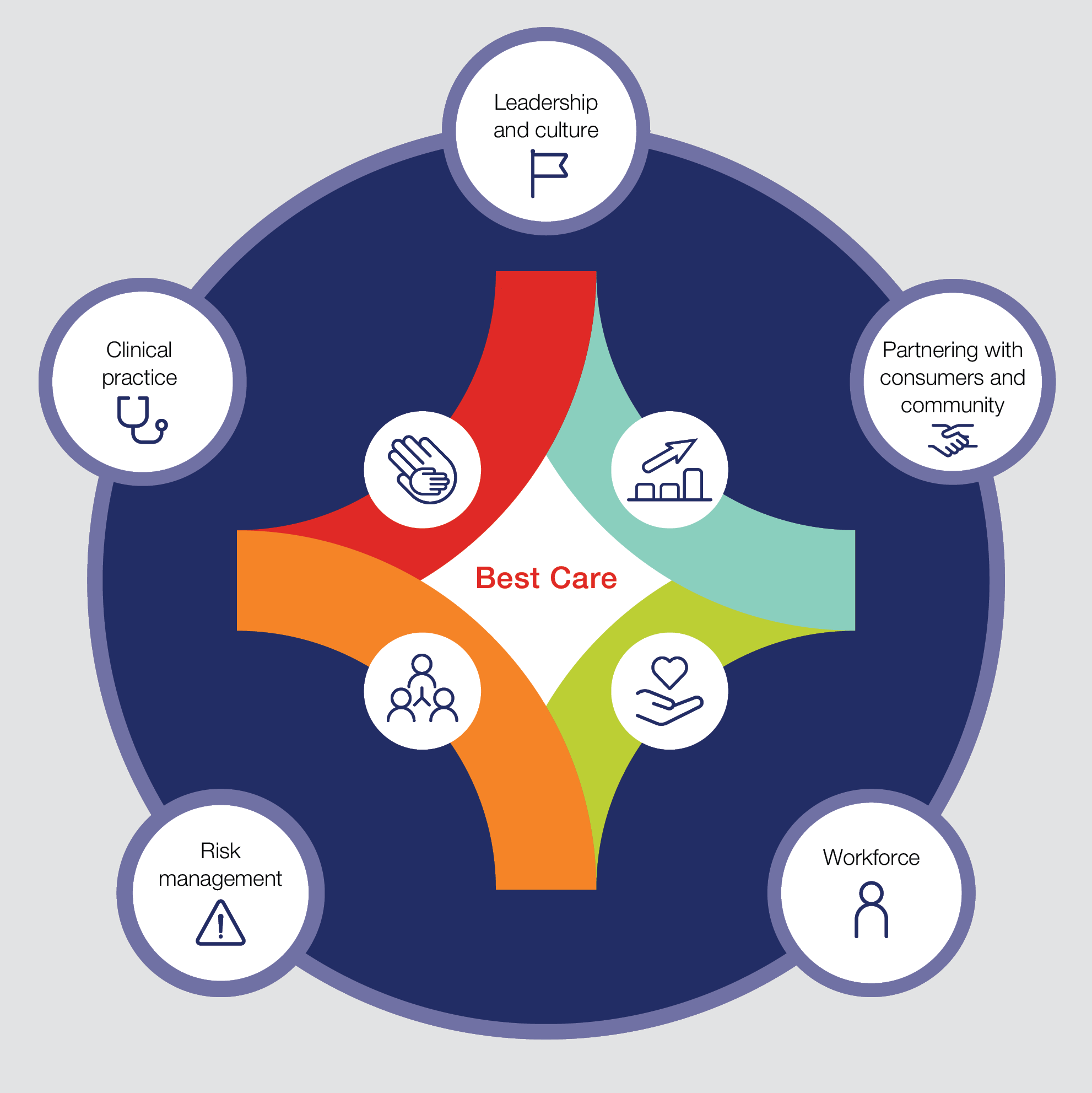
To ensure all patients receive best care, improved health outcomes and experience, in 2024-25 we launched the Best Care, Everywhere framework, which outlines our shared commitment to safe, effective, person-centred and connected care.
We commenced embedding the new Standards for Safe and Timely Ambulance and Emergency Care for Victorians into operational practice and we continued to work with health services to progress the Timely Emergency Care Program (TEC2), which provides a consistent approach to quality improvements.
The Additional Mobile Intensive Care (MICA) paramedics initiative saw the commencement of Bairnsdale single responder units, and critical care liaison paramedics helped to establish an enhanced framework for critical care and clinical support to better identify and treat critically unwell patients across the health system.
In 2024-25 we continued to increase service accessibility by pioneering the first paramedic practitioner role in Australia, alongside our partners the Department of Health (DH) and Monash University.
Impact
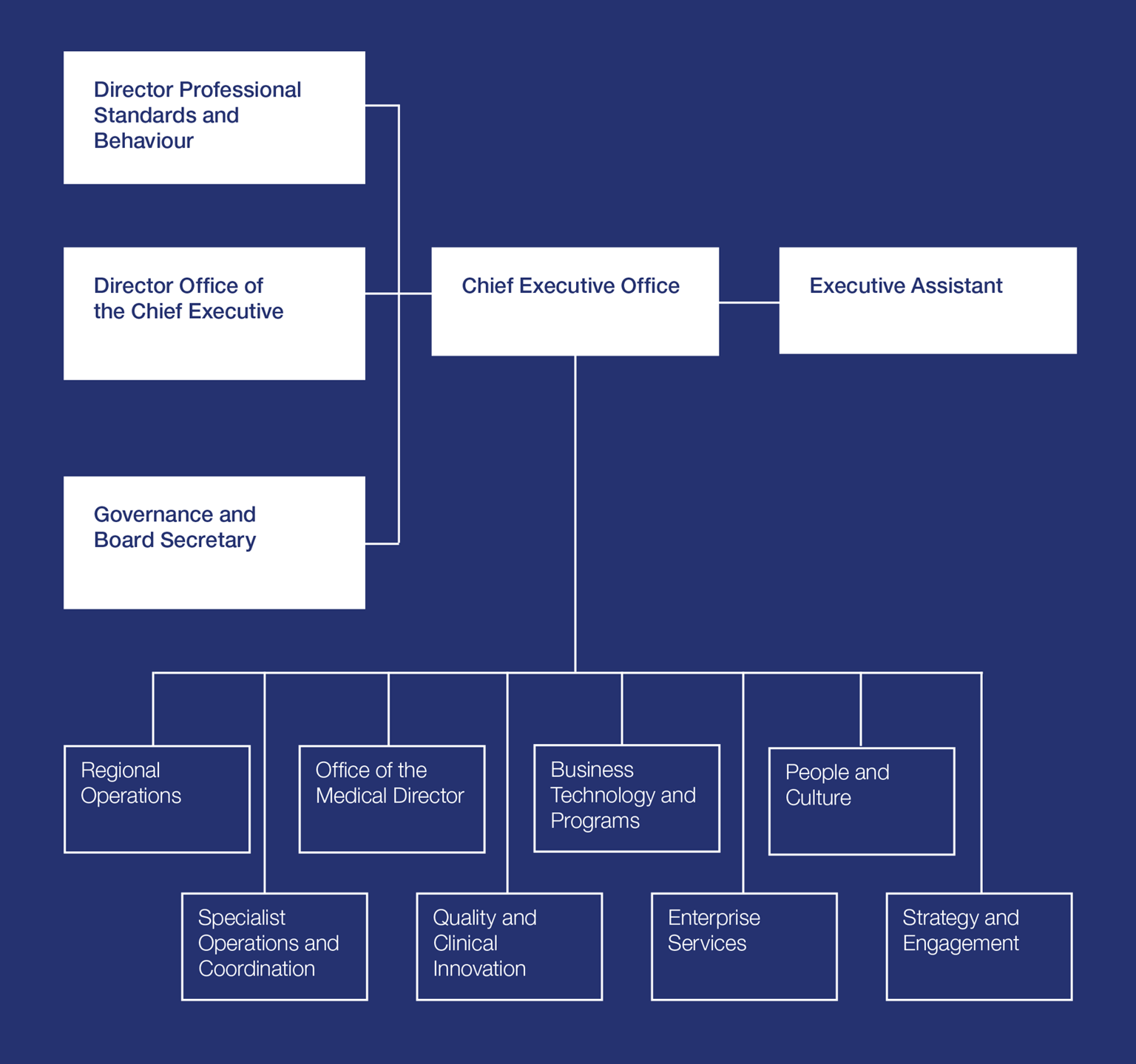
The Impact pillar aims to evolve our structure, processes, systems and assets to deliver more impact through consistent organisational performance.
In 2024-25 we transitioned to a more efficient and modern organisational model by issuing more than 5,000 personal iPad devices to in-field paramedics. We also upgraded VACIS to ensure paramedics could collate, manage, review, and report on patient care, paramedicine and clinical practices, and undertake clinical research.
Through the year we rolled out new digital radios across rural regions to support the Digital Radio Upgrade Program (DRUP2), which will enable compatibility between metropolitan Melbourne and other regions to deliver a single, secure radio network for Victoria.
This year our Secondary Triage team expanded the use of Video Assisted Triage (VAT), enabling us to better assess a patient’s condition and determine the best medical care options for them.
Connection
The Connection pillar aims to ensure we are seamlessly connected to each other, our patients, our partners and to the healthcare system; enabled through deeper engagement, research and advocacy, innovation and co-design, digital enablement and data sharing.
In 2024-25 we completed the implementation of our ‘Reflect’ Reconciliation Action Plan (RAP) and have developed our ‘Innovate’ RAP which will begin implementation in 2025-26.
We continue to promote and use the Victorian Virtual Emergency Department (VVED) via our Secondary Triage and in-field paramedics to more effectively connect patients to the right care.
We introduced regional community forums in 2024-25 which provide an opportunity for Board, Executive, Community Advisory Committee and local AV leadership to connect with communities at a local level and directly hear the needs and views of ambulance users and communities.
Strategic enablers
Innovation
Expanding and integrating innovation into all practices across the organisation.
Digital
Embracing digital technologies to improve patient care, operational efficiency, communication, collaboration, and innovation.
Research
Conducting research to improve patient care, inform evidence-based decisions, and develop new services and solutions.
Sustainability
Reducing environmental impact, developing sustainable business models, and future-proofing operations.
Declarations and attestations
Responsible Body Declaration
In accordance with the Financial Management Act 1994, I am pleased to present the Report of Operations for Ambulance Victoria for the year ended 30 June 2025.
Andrew Crisp
Chair of the Board
Melbourne
6 October 2025
Financial Management Compliance Attestation Statement
I, Amanda Watt, on behalf of the Board, certify that Ambulance Victoria has no Material Compliance Deficiency with respect to the applicable Standing Directions under the Financial Management Act 1994 and Instructions.
Amanda Watt
Chair of the Audit and Risk Committee
Melbourne
6 October 2025
Data Integrity Declaration
I, Jordan Emery, certify that Ambulance Victoria has put in place appropriate internal controls and processes to ensure that reported data accurately reflects actual performance. Ambulance Victoria has critically reviewed these controls and processes during the year.
Jordan Emery
Chief Executive Officer
Melbourne
13 October 2025
Integrity, Fraud and Corruption Declaration
I, Jordan Emery, certify that Ambulance Victoria has put in place appropriate internal controls and processes to ensure that integrity, fraud and corruption risks have been reviewed and addressed at Ambulance Victoria during the year.
Jordan Emery
Chief Executive Officer
Melbourne
13 October 2025
Conflict of Interest
I, Jordan Emery, certify that Ambulance Victoria has put in place appropriate internal controls and processes to ensure that it has complied with the requirements of hospital circular 07/2017 Compliance Reporting in Health Portfolio Entities (Revised) and has implemented a ‘Conflict of Interest’ policy consistent with the minimum accountabilities required by the VPSC.
Declaration of private interest forms have been completed by all Executive staff within Ambulance Victoria and members of the Board, and all declared conflicts have been addressed and are being managed. Conflict of interest is a standard agenda item for declaration and documenting at each Board and Board Committee meetings.
Jordan Emery
Chief Executive Officer
Melbourne
13 October 2025
A year in numbers
Performance
- 393,671
- time-critical code 1 cases attended
- 15 mins 29 secs
- State-wide average response time to code 1 cases
- 98%
- of patients reported good or very good experiences
- 35,092
- patients were seen using Video Assisted Triage by AV clinicians
- 5,157
- Victorian Stroke Telemedicine (VST) consultations
People
- 229
- New paramedics welcomed to AV
- 71
- New first responders
- 13
- New branches opened in 2024-25
Research impact
- 105
- active research projects
- 76
- peer-reviewed publications
- 11
- new research agreements
- 2,404
- citations in peer-reviewed literature
- 48
- citations in policy or scientific statements
- 32
- conference presentations
Emergency Management Unit events
July 2024
Traffic incident in Saw Mill Settlement
July 2024
Chemical factory fire in Derrimut
August 2024
Traffic incident in Koo Wee Rup
October 2024
Complex traffic accident Dargo
October 2024
Hazmat incident Tangill South
December 2024
Bushfire The Gurdies
December 2024
Bushfire Grampians National Park
January 2025
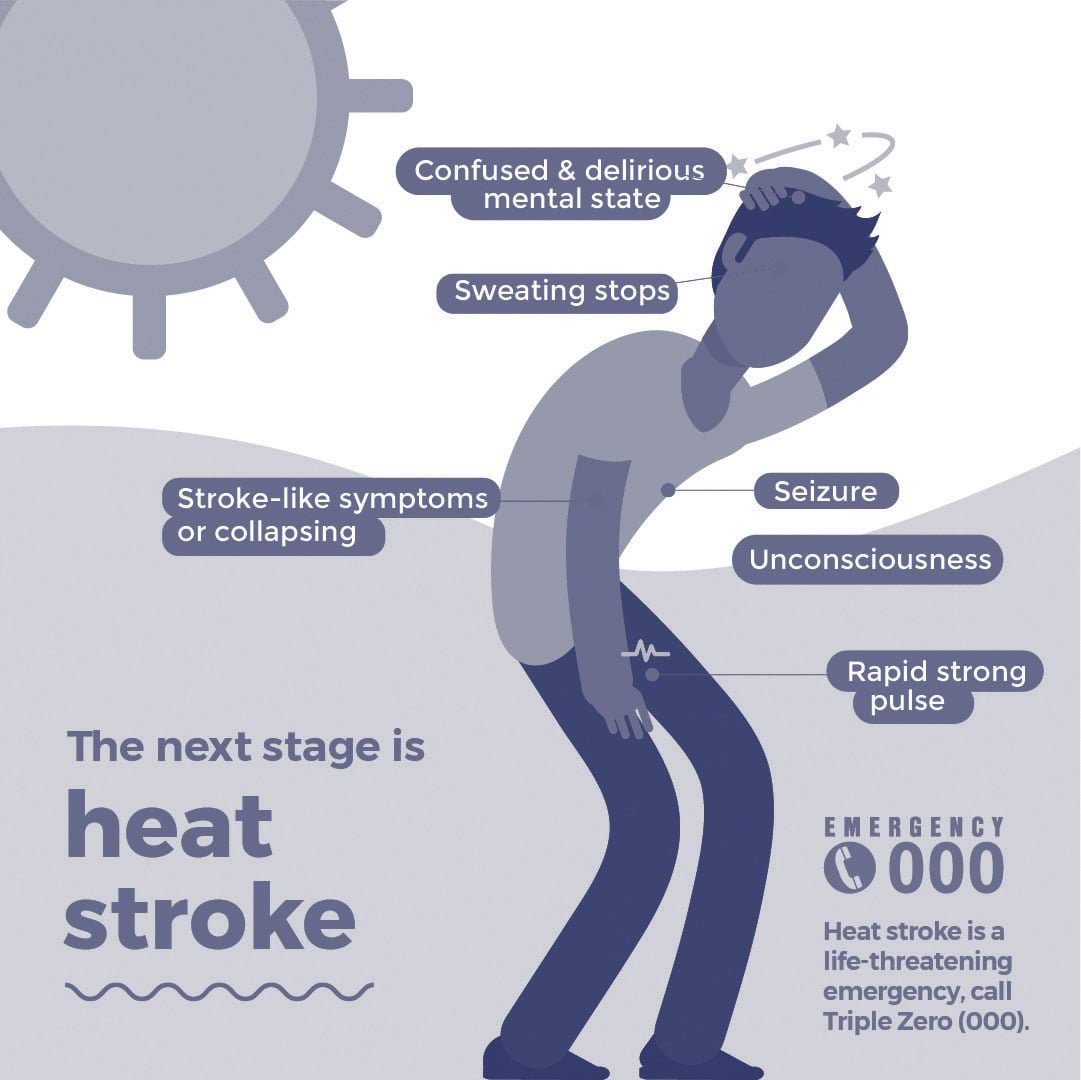
Severe heatwave statewide
January 2025
Bushfire Little Desert National Park
January 2025
Lithium battery factory fire Highett
February 2025
Wilderness response Taggerty
February 2025
Wilderness response Mt Buller
March 2025
Wilderness response Mt Buller
March 2025
Grass fire Trafalgar East
March 2025
Grass fire Montrose
March 2025
Hazmat incident Coldstream
March 2025
Hazmat incident Barwon
April 2025
House fire Mildura
May 2025
Industrial fire Springvale
May 2025
Wilderness response Iguana Creek
June 2025
Hazmat incident Broadmeadows
Membership Subscription Scheme
- 2.758m
- people covered
- 1.355m
- membership policies
- 74,600
- new memberships
- $106.24m
- direct revenue provided
- 174,740
- transports
- 97.63%
- customer satisfaction
- 365,758
- direct interactions with the contact centre
- 314,000
- phone calls
- 12,312
- online chats
- 44,214
- emails and letters
Our people
Improving the experience of our people at work has remained at the heart of several innovative programs and strategic initiatives undertaken over the past year. We have prioritised outcomes that ensure our people are well-supported, trained and connected to leadership and each other, including the appointment of key frontline leadership positions to support our people and provide leadership stability.
Major initiatives have included the delivery of a new enterprise agreement for our operational teams, the development of the Paramedic Practitioner Program, the introduction of Employee Engagement Forums for Regional Operations, and comprehensive health, safety and wellbeing measures to keep our people safe.
We recognise that while we have made some significant steps towards building our respectful and safe workplace, our long-term change journey continues, with the delivery of key initiatives under the new People Plan a key focus for the coming year.
Ambulance Victoria Enterprise Agreement (AVEA) finalised
The AVEA 2024 became operational on 21 February 2025, marking an important milestone for our organisation and our people covered under the agreement. Spanning the next four years until 2028, the AVEA 2024 reflects our ongoing commitment to creating a more fair, safe and inclusive workplace. Reaching this outcome was the result of strong collaboration and sustained dialogue with our workforce and representative bodies over many months including our union partners: the Victorian Ambulance Union (VAU) and the United Workers Union / Ambulance Employees Australia Victoria (UWU/AEAV).
A number of improvements to terms and conditions of employment are contained in the AVEA 2024.
Key improvements relate to salary increases, classification updates and backpay, as well as End of Shift (EOS) arrangements, and further recognition of our Ambulance Community Officer (ACO) cohort, as well as those translating across to the Ambulance Victoria (Management and Administrative Staff) Enterprise Agreement 2021 (AVMA 2021) from the AVEA 2024.
Importantly, the AVEA 2024 not only addresses current workplace needs but also positions us for long term success. By strengthening our Agreement, we are better equipped to attract and retain top talent, drive engagement, and foster a high performing culture.
Bargaining for the Ambulance Victoria (Management and Administrative Staff) Agreement (AVMA) 2025 commenced in April 2025 and remains underway.
Paramedic Practitioner Program
AV is a key partner alongside DH and Monash University in pioneering the first paramedic practitioner role in Australia. A paramedic practitioner is a highly skilled and specialised paramedic with advanced training in primary healthcare. They can assess, treat, and manage a wide range of health conditions, often working in collaboration with doctors, nurses, and other healthcare professionals. Paramedic practitioners can provide care in various settings, including GP surgeries, community health centres, hospitals, and even in patients’ homes.
The first cohort of 28 paramedics are currently undertaking their second year of the nation-leading paramedic practitioner master’s degree at Monash University – with a second cohort of 26 students commencing in February 2025.
Developed alongside AV, Safer Care Victoria (SCV), paramedics, clinicians, and unions, the first cohort of paramedic practitioner graduates will be deployed to regional Victoria in 2026.
Once graduated, they’ll be able to treat conditions that commonly see people visit a hospital – including urinary catheter care, wound care and closure, minor infections, dislocations and fractures.
This year, they commenced clinical placements at nine health services across Victoria to consolidate their advanced course learnings and skills. A key milestone for the new paramedic practitioner role was the amendment to the Drugs, Poisons and Controlled Substances Act 1981 this year which has paved the way for them to prescribe and administer scheduled medicines, treat patients on the spot and reduce the need to transport to hospital.
In February 2025, a new cohort of 26 paramedic practitioner students commenced their three-year course, expanding the number of overall people who will soon be available to step into advanced practitioner roles.
We continue to work closely with the Chief Paramedic Officer, SCV, DH, Monash University and others to help design this innovative role to best suit future needs.
Key statistics
Cohort 1
30 students, commenced their studies in 2024, clinical placement in 2025.
Cohort 2
26 students, commenced their studies in 2025, clinical placement from 2026.
Employee Engagement Forums
The AVEA 2024 marked the formal introduction of Employee Engagement Forums (Clause 19 on page 30) for the operational workforce.
AV’s Strategy and Engagement division and Regional Operations division (RO) worked together to develop a plan to implement these forums from March 2025 onwards, beginning first with operational staff before rolling out to the broader, non-operational working in June 2025 where they are referred to as ‘Town Halls’.
A key part of these gatherings it to ensure the key themes, issues, outcomes and actions are captured and reported on to support an organisational response and increase the opportunities for our people to give feedback on their experience at work.
Area Managers have since shared those key themes, issues, outcomes and actions with their entire region so that issues raised in meetings are being addressed at a local leadership level.
In March 2025, key themes consistently raised across the 26 areas related to issues with our rostering system, iPad ergonomic concerns, lack of availability of short night shifts, and delays to addressing payroll requests and support tickets.
Although forums are not new to AV, the introduction of Employee Engagement Forums and divisional Town Halls simply formalises the meeting frequency and provides a structure to support our people to have a local avenue to raise their questions and concerns, to support leaders in hosting those meetings and to provide a mechanism for them to report back on the issues raised and the actions taken as a result.
YourAV: Building our safe and respectful workplace
In January 2025, the Victorian Equal Opportunity and Human Rights Commission (the Commission) released its final progress report outlining AV’s implementation of 25 priority recommendations, made as part of the 2022 Independent Review into Workplace Equality in Ambulance Victoria.
The Commission acknowledged key achievements that are making a difference – with a focus on the establishment of a dedicated Professional Standards and Behaviours Department and defined pathways for reporting harmful behaviours.
The Commission also provided a series of enablers and barriers to change, to help guide us in refining our approach going forward. These insights, which were informed by our people’s stories and experiences, give us a deep understanding of the next steps in creating an AV that is safe, fair and inclusive for everyone.
A comprehensive review process has taken place to determine the next steps for the program. Many initiatives have now been delivered and closed, while ongoing initiatives have been integrated into our core business activities and systems.
Improving our people’s experience at work
Some recommendations from the Commission that are still underway have been integrated into our new People Plan – a three-year plan dedicated to improving the workplace experience for our people – such as our continued focus on building leadership capability, and the organisation-wide delivery of Upstander, a dedicated education program to help our people speak up about harmful behaviours at work.
The People Plan sets out the key actions AV will undertake to improve our people’s experiences at work and while volunteering at AV. Developed in response to feedback from across the workforce, the People Plan addresses four key outcomes:
- We are diverse, meaningfully engaged and valued.
- We are safe, healthy and we care for everyone.
- We are capable and continuously learn and grow.
- We consistently develop effective leadership.
Implementation of the People Plan will be monitored against key performance indicators, drawing on data from a range of sources, including feedback from the workforce, unions and People Matter surveys. Progress will be shared regularly as the various projects are implemented, with a detailed progress report shared annually.
Wellbeing and support services
The Mental Health and Wellbeing Action Plan 2022–2025 marked AV’s third strategic framework dedicated to supporting the psychological health of our workforce. In 2024-25, we successfully completed all outstanding actions across the plan’s 17 projects, each aligned to four key pillars: Prevention and Education, Early Intervention, Building on Strengths and Partnering for Success.
During the year, we released the results of our biennial psychosocial survey, a key initiative aimed at understanding the evolving mental health and wellbeing needs of our workforce. The 2024 survey saw a strong increase in engagement, with 22.8 per cent of employees responding – more than double the response rate from 2021.
The findings revealed encouraging trends, with overall reductions in reported symptoms of anxiety, stress, and depression compared to previous years. These improvements suggest that our continued investment in prevention and early intervention programs is making a meaningful difference.
However, the survey also highlighted areas of concern, particularly around post-traumatic stress disorder (PTSD) and burnout, which remain prevalent across the workforce. These insights will play a critical role in shaping future initiatives, enabling our Wellbeing Support Services (WSS) team to tailor support programs that respond directly to the needs of our people.
The next psychosocial survey is scheduled for 2026, continuing our commitment to evidence-based wellbeing strategies.
Consultation for the next iteration of the Mental Wellbeing Action Plan was also completed this year and the upcoming 2025–2028 plan will focus on:
- Improving access to mental health and wellbeing services.
- Embedding support across all levels of the organisation.
- Evaluating outcomes to ensure programs deliver meaningful impact for our people.
Key statistics
- In 2024-25, 63.5 per cent of the workforce accessed support through WSS.
- Suicide Intervention Response and Engagement Network, our in-house bespoke suicide prevention package, was voluntarily completed by over 60 per cent of the workforce (> 5000 people) with 96.5 per cent reporting it beneficial for their role at AV.
- Our VACU network continues to expand with 131 clinicians providing care across the state.
- Our 24/7 counselling line received 447 calls, offering confidential support for staff, volunteers, families and retirees. AV continues to partner with Victorian Council of Churches Emergency Ministries for coverage across the state of Victoria in pastoral care with 17 volunteers and AV chaplains visiting branches and hospitals.
- The Peer Dog program made 561 site visits, helping reduce stigma around mental health.
- Peer Support team welcomed 29 new volunteers, bringing the total Peer Support responders to 225.
Advance allocation process
AV is proud to have implemented the Advance Allocation Process (AAP) to strengthen workforce stability and enhance employee satisfaction, both of which are central to the high-quality care AV provides to communities across Victoria. The AAP represents a thoughtful, people-centred shift in workforce planning, balancing operational needs with employee wellbeing and community care.
Under this model, Graduate Ambulance Paramedics (GAPs) are provided with a permanent work location as part of the offer of employment, rather than at the end of their graduate year. This approach empowers new recruits with greater autonomy and certainty, enabling them to make informed decisions about their future career.
For employees, the AAP significantly reduces the stress and financial burden associated with relocation, fosters stronger community ties, and improves overall job satisfaction. Operationally, the AAP supports proactive workforce planning to enable better resourcing decisions, particularly in remote and hard-to-fill locations, ultimately enhancing service delivery for patients in the community. By aligning employee preferences with organisational needs, the AAP strengthens recruitment and retention strategies and promotes a more engaged and resilient workforce.
Building on its success, the AAP is being extended to include the MICA workforce. This marks a significant step in AV’s commitment to a people-focused approach – one that thoughtfully balances operational priorities with the wellbeing of our employees and the needs of the communities we serve.
What our workforce is saying
This gives graduates far more stability and is a great process to prevent movement after becoming established in an area.
This is a wonderful piece of work and a true commitment to making this a great place to work and volunteer. Kudos for listening and responding: this will mean a lot, to a lot.
This change gave our team the confidence to prepare and welcome our new staff early, instead of scrambling last minute.
Best Care for People with Communication Disability Project
The launch of the Best Care for People with Communication Disability Project demonstrates AV’s excellence in leadership in creating a communication accessible service, recognised by the Council of Ambulance Authorities. An impactful five-year partnership with Scope Australia has delivered workforce training and resources designed to bridge communication gaps between paramedics and the one in seven patients who experience communication difficulty.
The resources, co-designed with people with lived experience and paramedics, ensure practical and effective application in health emergencies. Easy English resources on AV’s website have been designed to empower community by increasing preparedness.
AV’s disability inclusion program continues to grow a network of champions across regions who are building awareness and understanding in Best Care with colleagues. This approach is increasing engagement with training and use of the Emergency Healthcare Communication Book with patients, as well as support for initiatives such as learning Auslan, reaching more than 5,500 ALS paramedics through our continuing education program.
The Best Care for People with Communication Disability Project has been made possible by a $1.9m National Disability Insurance Scheme’s Information, Linkages and Capacity Building Grant.
Best Care is about creating a healthcare environment where people with communication disability can feel heard, understood and respected. These resources will not only help emergency workers communicate more effectively but will also provide patients with the confidence to express their needs clearly during what can be an overwhelming time.
Paramedics during discovery phase
I have never felt completely informed or prepared to assist patients with specific disabilities that are medically unwell. Twenty-two years in ambulance gives you some experience and knowledge, but I have never felt informed, comfortable or at ease when managing and caring for this cohort of patients.
I often feel like I haven’t done the best job advocating for the patient… I would definitely like some training as I feel like I’m winging it most of the time.
Parliamentary Inquiry
On 14 August 2024, the Legislative Council agreed that the Legal and Social Issues Committee (the Committee) inquire into, consider and report on the core issues impacting the management and functions of Ambulance Victoria, including but not limited to:
- issues involving call-taking, dispatch, ambulance ramping, working conditions and workloads of paramedics;
- procurement practices, including contract management and oversight, and their adequacy in ensuring transparency, fairness, and value for public funds and identification of any systemic patterns of mismanagement or lack of oversight;
- allegations of fraud and embezzlement and the adequacy of financial controls and oversight to prevent misconduct;
- governance and accountability;
- the workplace culture within Ambulance Victoria, with a focus on occupational health and safety impacts, including to the morale and wellbeing of paramedics and employees; and
- any other related matters the Committee considers relevant.
AV’s submission to the Committee provides a comprehensive overview of our organisation, its history, governance, funding and the types of services we provide. It demonstrates our commitment to working with our healthcare partners to address whole of health system problems and the need for a whole of health system solution.
The Committee held several public hearings with evidence from AV, as well as public and private parties and individuals. The Committee will review the evidence provided through the hearings and the submissions. A final report for Parliament is due by 14 October 2025.
AV continues to engage with the Inquiry with a genuine desire to improve, and in a manner that is open, transparent and honest on responding to the Committee’s report.
Clinical advancements
Our dedication to clinical excellence drives us to continuously innovate and improve our healthcare services. From world leading out-of-hospital cardiac arrest survival results, to a robust Medical Directorate keeping abreast of contemporary guidelines, to comprehensive educational programs and international partnerships, our clinical advancements are at the national forefront of transforming healthcare.
Our Victorian Ambulance Cardiac Arrest Registry results
Victoria has Australia’s best cardiac arrest survival rate and the third best in the world, following a record year as reported in the Victorian Cardiac Arrest Registry (VACAR) Annual Report.
Bystander cardiopulmonary resuscitation (CPR) was administered in 79 per cent of witnessed cases and 141 cases receiving a shock from a public Automated External Defibrillator (AED) – the highest number on record. As a result of these interventions, and the dedication of paramedics and first responders, 422 people who had experienced an out-of-hospital cardiac arrest were discharged from hospital, with 84 per cent returning home to their families.
With our highest internationally comparable survival rate, 41 per cent of patients survived to hospital discharge. The rise from 36 per cent in 2022-23 marks the largest annual increase in the past decade and is a testament to the efforts of all at AV.
These improvements in survival are not by chance – they reflect the unwavering dedication of our paramedics and first responders, the responsiveness of the community, and the targeted initiatives that have strengthened the chain of survival.
The Ambulance Victoria Cardiac Arrest Improvement Strategy 2023-28 continues to drive innovation in emergency response. In 2024-25, we continued the FIRST: First Responder Shock Trial alongside St John New Zealand to help GoodSAM responders use defibrillators more often when assisting patients.
The trial in Victoria and New Zealand has been running since 2022 and provides GoodSAM responders with a CellAED (Update January 2026: The Therapeutic Goods Administration has issued a Critical Recall for all lots of the CellAED devices).
This device is a small portable defibrillator. The trial will determine if this device can help more people survive 30 days after a cardiac arrest outside of hospital. It will also determine if this can be a method for the public to provide help sooner when someone’s heart stops.
Additionally, the expansion of the Heart Safe Communities program has introduced 12 new communities this year.
With 17,327 GoodSAM responders now registered, and 10,304 AEDs available across Victoria, community involvement in cardiac arrest response continues to grow.
Leading clinical excellence
The Office of the Medical Director (OMD) serves as AV’s clinical leadership hub, overseeing the development, implementation, and continuous refinement of Clinical Practice Guidelines (CPGs) and procedures that ensure paramedics, first responders, nurses, and doctors deliver safe, evidence-based, and contemporary clinical care to the Victorian community.
The OMD delivered several critical guideline updates throughout 2024-25, each designed to enhance patient outcomes and clinician safety. In October 2024, the first major CPG update introduced revised acute behavioural disturbance guidelines that better balance optimal patient care with paramedic safety considerations. Three new guidelines were also launched, all addressing critical gaps in clinical guidance:
- Withholding or Ceasing Resuscitation (paediatric)
- Sepsis and infection (adult and paediatric)
- Clinical Care Outside Scope of Practice
November 2024 saw the introduction of new clinical work instructions for stacked shocks, while March 2025 brought significant changes to intranasal fentanyl administration protocols. These updates, alongside targeted enhancements for Adult Retrieval Victoria (ARV) and wilderness paramedics, ensure AV’s clinical practices remain at the forefront of emergency medical care.
Improvement and innovation
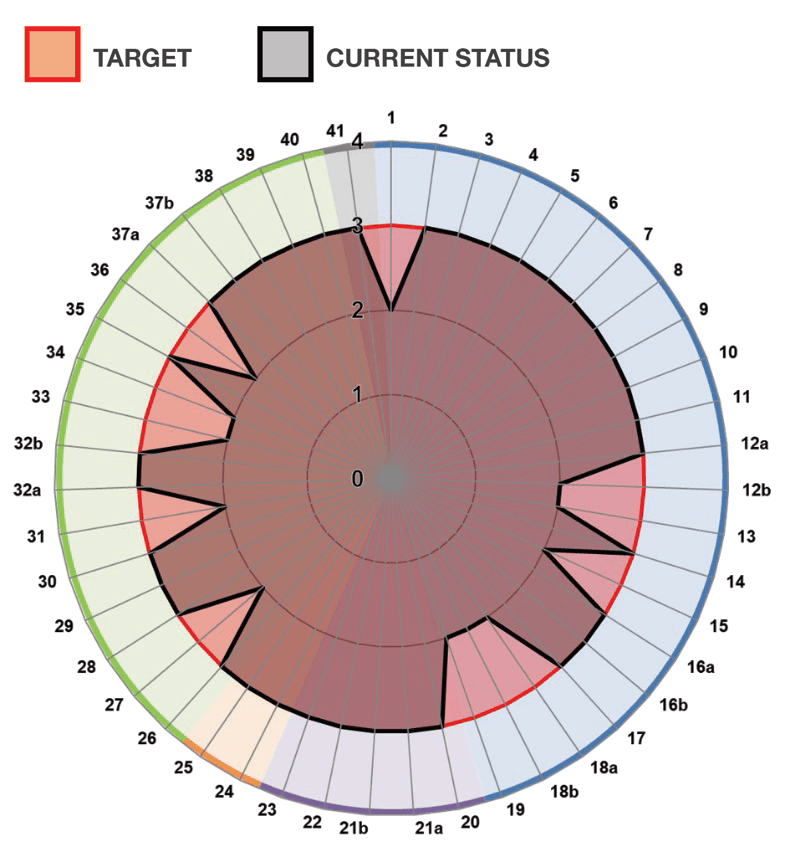
The Standards for Safe and Timely Ambulance and Emergency Care for Victorians
The DH Standards for Safe and Timely Ambulance and Emergency Care for Victorians (the Standards) seek to improve whole-of-hospital flow so that patients arriving via ambulance can be consistently transferred to the care of a hospital in a timely manner.
It involves AV and our health service partners working together to meet new benchmarks for efficient transfers, clearing times, alternative care pathways, and hospital coordination. There are 10 Standards in total, and five where AV has a detailed role.
Our work towards meeting the Standards includes embedding clear processes, communicating and engaging with our people about strategies, improving reporting frameworks and aligning AV’s operational practices with system-wide healthcare goals.
We are also testing and refining care models through the Timely Emergency Care 2 (TEC2) project (read about TEC2 in the next section).
In improving our response performance and getting ambulances back out on the road more efficiently, we are best placed to deliver best care to our Victorian community.
Timely Emergency Care 2
Launched in September 2024, the TEC2 program is a partnership between AV, DH, and the Institute for Healthcare Improvement (IHI).
The program aims to embed a consistent, evidence-based approach to quality improvement across AV, and is also contributing to our work towards the Standards (as outlined in the section above).
Multidisciplinary teams comprising of staff who work directly with patients have been using the Model for Improvement framework to develop and test change ideas in real-world settings. The objective is to learn quickly, implement effective solutions, and scale successful initiatives across Victoria to improve efficiency and ensure timely access to care.
Focus areas and opportunities for TEC2 have been informed by engagement across our workforce. In total, 155 staff from a range of roles and locations engaged via survey or in-depth interview. Four key themes were identified:
- Effective call taking and dispatch ensures emergency ambulances are available for patients with higher acuity needs.
- Optimising alternate pathways and supporting care being provided in place, virtually and outside emergency departments would reduce avoidable hospital transports.
- Timely handover at hospitals – helping paramedics get back on the road.
- Resourcing and process improvements to maximise efficiency, enhance wellbeing and improve ambulance availability.
Priority projects were identified across four focus areas: Daily Operating System, Transfer, Clearing, and Safe in Place (in field). Change teams, comprised of members from the operational workforce, were established and supported by a capability program co-designed and delivered in partnership with DH and IHI.
In 2024-25, 53 AV staff participated in one or more TEC capability sessions – including leadership, operations and corporate roles.
Early promising results were seen at Box Hill Hospital, Ballarat Hospital, Goulburn Valley Health, and Sunshine Hospital, where updated clearing and transfer practices were tested as part of TEC2. Improved transfer and clearing times were demonstrated through earlier ePCR initiation, leadership presence in EDs and targeted communication to operational teams. This also includes the team-based approaches, such as ‘stride or ride’, or hospital-based approaches, such as the workstation-on-wheels.
Work will continue to drive continuous improvement across the four identified priority areas. In addition, efforts are now focused on developing a sustainable model to scale and embed the improvement capability established through TEC2.
This model will be utilised to support further implementation of performance standards and other strategic initiatives aligned with the delivery of timely and high-quality patient care.
TEC2in action
Workstation-on-wheels involved trialling two mobile, ergonomic iPad workstations (‘Paramos’) at Box Hill Emergency Department to support timely electronic patient care record (ePCR) completion during patient transfer, aiming to reduce documentation delays, improve paramedic workflow, and enhance hospital clearing efficiency.
Stride or Ride has been tested at Box Hill Hospital and is about encouraging patient movement into the emergency department via walking or wheelchair, where it is safe and practical. This helps support better offload times for AV crews and helping them to get back on the road and attending to emergencies sooner.
Safer Together Program
The Safer Together Program is Safer Care Victoria’s (SCV) statewide safety improvement initiative. It aims to build a continuously learning and improving health system that is safer, more person-centred, sustainable, and delivers better outcomes for all Victorians.
Through our participation in this program, AV has collaborated with SCV and the broader health sector to:
- Design, implement and evaluate quality improvement projects.
- Share insights, findings and resources.
- Contribute to the development of a learning health system.
AV is currently participating in the collaborative streams of the Victorian Sepsis Program and the Enhancing Stroke Care Collaborative. These initiatives bring together AV, SCV and health services to improve the quality of sepsis and stroke care across the state through shared learning and coordinated action.
Adult Retrieval Victoria
Adult Retrieval Victoria (ARV) provides statewide critical care clinical advice and coordinates the transfers of critically unwell patients from across the state. In addition to these core functions, ARV is a central part of the state trauma system, supporting the retrieval coordination of major trauma patients as well as providing clinical expertise.
In 2024-25, our multidisciplinary team of doctors, critical care nurses, patient transport officers and retrieval administrative support officers coordinated the care of 7,131 patients, including 52 patients on heart-lung bypass, or extracorporeal membrane oxygenation (ECMO).
This year has seen our team have access to a bespoke complex patient ambulance vehicle that can accommodate the most complex of our patients, including those that are on ECMO and balloon pump support.
Our ongoing pivotal role in the pre-hospital intensive care unit (ICU) bypass initiative allows MICA paramedics to work with ARV to balance the load between ICUs and prevent secondary transfers due to lack of bed availability.
Our expert team of skilled and efficient retrieval administrative support officers, who field on average 610 calls per day, also additionally answer all calls for the Victorian Extracorporeal Membrane Oxygenation Service, as well as all calls for the VST service after hours. June 2024 was our busiest month ever with 21,584 calls to our team for assistance.
Adult retrieval snapshot
- 222,850
- calls received
- 7,131
- cases*
- 4,534
- retrievals
- 1,246
- medical retrievals**
- 52
- ECMO transfers
- 1,065
- pre-hospital cases
- 15
- clinical authorisation cases
- 137
- pre-hospital ICU bypass
* Cases refer to all referrals made to ARV.
** Retrievals refer to all patients transported under the care of ARV (any skill set). Medical retrievals are those retrievals performed by an ARV doctor (consultant or registrar).
| Region | Total cases | Air retrievals | Road retrievals |
|---|---|---|---|
Barwon South West | Total cases 758 | Air retrievals 263 | Road retrievals 495 |
Gippsland | Total cases 1,167 | Air retrievals 360 | Road retrievals 454 |
Grampians | Total cases 573 | Air retrievals 120 | Road retrievals 242 |
Hume | Total cases 1,207 | Air retrievals 577 | Road retrievals 206 |
Loddon Mallee | Total cases 1,114 | Air retrievals 525 | Road retrievals 262 |
Metro | Total cases 1,826 | Air retrievals 6 | Road retrievals 1,238 |
Our research
AV’s Centre for Research and Evaluation is an international leader in pre-hospital emergency care, health services and resuscitation research.
Between July 2024 and June 2025, 105 active research projects were registered in the AV research governance system and staff led or contributed to the publication of 76 peer-reviewed manuscripts, many in high-impact and top-ranking journals in fields of emergency medicine, cardiology, and pre-hospital emergency care.
Our research program is internationally recognised, attracting almost 2,500 citations across peer-reviewed literature in 2024-25, including 48 citations in policy and scientific statements or treatment guidelines. Our research is highly collaborative, involving partnerships with universities, hospitals, and research institutions. In 2024-25, we proudly signed 11 new research agreements with partners, helping us achieve our strategic goal of being a strong, connected, and collaborative research centre.
Highlights
Smartphone alerts boost survival after cardiac arrest
A study led by AV found that smartphone-activated volunteer responders could play a crucial role in saving lives after cardiac arrest.
The research, published in the Medical Journal of Australia, analysed 9,196 adult out-of-hospital cardiac arrests between 2018 and 2023 and looked at the impact of volunteers alerted through the GoodSAM smartphone application. Volunteer responders attended 13 per cent of eligible cases, arriving before paramedics in nearly half of them.
When volunteer responders arrived before paramedics, the chances of someone receiving CPR were more than seven times higher, and the chances of early defibrillation were about 16 times higher. Importantly, the likelihood of survival to hospital discharge also improved by 37 per cent compared to when no volunteer responders attended cardiac arrests. The study indicated that expanding smartphone-based programs across Australia and increasing the number of trained volunteers could significantly increase survival rates from cardiac arrest.
Paramedics deliver antibiotics early in ground-breaking sepsis trial
In a first-of-its-kind Australian trial, paramedics in Victoria collected blood cultures and administered intravenous antibiotics before hospital arrival in patients suspected of having sepsis (i.e. a severe blood stream infection). The results, published in Emergency Medicine Australasia, show promising potential for accelerating the early treatment of sepsis.
The Paramedic Antibiotics in Severe Sepsis (PASS) trial enrolled 35 adults showing signs of infection, low blood pressure, and altered consciousness. All had blood cultures drawn by paramedics, with 89 per cent successfully collected and 42 per cent of which confirmed infection.
Participants were randomly assigned to either standard care or standard care plus two grams of intravenous ceftriaxone administered by paramedics. Patients who received antibiotics by paramedics got treatment 108 minutes faster than patients in the control group (median time: 42 min vs 150 min.
The study confirms that paramedics can safely perform advanced procedures like blood culture collection and intravenous antibiotic delivery in the field. While the PASS trial marks an important step in bringing hospital-level sepsis care to the roadside, larger trials are needed to determine whether earlier therapy improves patient outcomes in severe sepsis.
Cultural barriers may limit the use of ambulances among multicultural communities
An AV study published in Pre-hospital Emergency Care has shown that people from culturally and linguistically diverse (CALD) backgrounds are significantly less likely to use ambulance services compared to other Australians. Analysing over 1.26 million cases between 2015 and 2019, researchers found that 21.6 per cent of ambulance patients were from CALD communities, yet their overall use of ambulance services was 13 per cent lower than non-CALD patients before accounting for demographic differences.
Once adjusted for age and gender, the disparity widened: CALD patients were 51 per cent less likely to call an ambulance compared to non-CALD Australians. The disparity was especially pronounced in certain emergencies – CALD patients were 61 per cent less likely to use ambulance services for mental health or substance-related crises compared to non-CALD patients.
The findings suggest that cultural, linguistic or social factors may prevent CALD individuals from seeking emergency care. Potential solutions could include community education, improving translation services, and culturally sensitive outreach – steps that could help ensure that everyone, regardless of background, has equal access to life-saving emergency care.
Victorian cardiac arrest survival rates triple thanks to bystander action
A new study led by AV shows that survival rates after cardiac arrest in Victoria have improved dramatically over the past two decades. Researchers analysed more than 102,000 out-of-hospital cardiac arrests recorded between 2003 and 2022 and found that while the overall number of cardiac arrests has remained steady, more people are surviving thanks to faster action from bystanders.
The study, published in the Medical Journal of Australia, showed that rates of bystander CPR increased from 40 per cent to 72 per cent over the 20-year period, while the use of publicly accessible defibrillators increased from less than one per cent to 16 per cent.
For patients whose cardiac arrest was witnessed and who had a shockable heart rhythm (known internationally as the ‘Utstein comparator group’), survival to hospital discharge was more than three times higher in 2022 compared with 2003.
Among survivors followed up a year after their cardiac arrest, about four in 10 reported a return to full health. The findings highlight the life-saving impact of teaching CPR, making defibrillators widely available, and encouraging members of the community to step in during a cardiac emergency.
Research funding
AV researchers were lead investigators of several new National Health and Medical Research Council (NHMRC), Medical Research Future Fund (MRFF) and National Heart Foundation (NHF) research grants in 2024-25. Research grants underpin our ability to invest in clinical innovation and support the critical infrastructure required to deliver world-leading clinical trials and cohort studies. In 2024-25, AV researchers and its research partners attracted over $8 million in research funding:
- Emergency Management Victoria Grant for ‘First responder and paramedics PTSD prevention through eye movement desensitisation and reprocessing: a randomised controlled trial. Funding: $374,505.
- Heart Foundation Catalyst Partnership Grant for ‘Transforming pre-hospital cardiac care: Getting the right treatment at the right time’. Funding: $100,000.
- NHMRC Centre of Research Excellence for ‘Improving the emergency response to save lives: An Aus-ROC Centre of Research Excellence’. Funding: $3,000,000.
- MRFF Cardiovascular Health Grant for ‘Improving outcomes and survivorship following sudden cardiac arrest in the young’. Funding: $4,999,576.
Awards
The Centre for Research and Evaluation received multiple awards in 2024-25 recognising its contribution to science in the field of pre-hospital emergency care. Associate Professor Ziad Nehme, Director of the Centre for Research and Evaluation, was awarded the 2024 NHMRC Peter Doherty Investigator Grant Award for Emerging Leadership, recognising him as one of Australia’s top emerging medical researchers.
Presented at the 2025 NHMRC Research Excellence Awards, the honour acknowledges his ground-breaking work in improving outcomes for cardiac arrest patients.
His research focuses on enhancing emergency call recognition, increasing bystander CPR and defibrillation through community engagement and technology, and improving post-resuscitation care to boost survival and neurological recovery.
In addition, paramedic Charlotte Kennedy was awarded the Best Free Paper Award at the 2025 ‘Spark of Life’ Conference in Melbourne, for a study examining the impact of the COVID-19 pandemic on CPR quality during cardiac arrest.
Finally, MICA paramedic and PhD candidate, Richard Armour, received the ‘Best Presentation from an Emerging Researcher’ award at the 2025 Monash Addiction Research Centre Symposium for his presentation titled ‘Initiation of opioid agonist therapy using buprenorphine in the emergency department or emergency out of hospital setting: A mixed-methods systematic review’.
These collective awards are strong acknowledgment of the impact of AV’s research.
Clinical Insights and Grand Rounds
In 2024-25, we continued to strengthen and evolve our clinical communication channels, with the continuation of Clinical Insights (publication) and Grand Rounds (clinical events).
This supports the sharing of knowledge, inspire reflection and foster informed dialogue across our clinical and operational workforce.
Launched the previous year, these initiatives centre around key clinical themes, offering in-depth exploration of topics including improving diagnosis for patient safety, trauma and mental health.
Through a refreshed approach, the 2024-25 series introduced broader subject areas, welcomed new contributors and created more opportunities for cross-disciplinary discussion and engagement.
These platforms remain focused on delivering content that is relevant, practical and grounded in real-world clinical experience, highlighting evidence-informed care, innovation and the stories that drive improved outcomes for patients and teams alike.
Best Care, Everywhere framework
In 2025, AV launched the second edition of its clinical governance framework, Best Care, Everywhere. This case study highlights a selection of resuscitation-focused initiatives demonstrating how the framework supports safe, effective, person-centred, and connected care for every patient.
- Safety and quality in resuscitation continue to be strengthened through a Safety-II lens and a culture of continuous learning.
- The new Out of Hospital Cardiac Arrest (OHCA) dashboard, developed by the VACAR team, enables targeted improvements using local cardiac arrest data.
- Expansion of our Secondary Triage team continues to ease pressure on emergency resources, while partnerships with Paediatric Infant Perinatal Emergency Retrieval, ARV and local hospitals ensure timely access to specialist expertise at the point of care.
- Neonatal response capability has been enhanced through the acquisition of preterm and real-time feedback mannequins, appropriate airway adjuncts and supporting effective team-based training.
- Updated clinical guidelines, including updated strategies for managing refractory ventricular fibrillation, support paramedics and first responders in applying best-practice care.
Person-centred care remains central to every resuscitation effort.
It’s reflected in our ongoing work to support and respect advanced health directives and end of life wishes.
Partnerships with the VVED and palliative care services enable timely, home-based symptom management. Strengthening our fire/emergency medical response partnerships and community engagement has broadened access to defibrillation and increased awareness.
Notification of survival to discharge ensures crews are informed when a patient they resuscitated survives to hospital discharge, acknowledging their care and reinforcing a vital feedback loop.
The collective, organisational wide efforts demonstrate the impact of a unified team and a cohesive clinical governance approach that gives every Victorian a greater chance of survival. Supported by the Best Care, Everywhere framework, and driven by commitment and accountability at every level, this coordinated work is saving Victorian lives.
It’s the ongoing, often unseen work that upholds, supports, and delivers the Best Care goals.
It’s people of all ages and backgrounds getting an increased chance of survival, because of the expertise, dedication and clinical leadership across every division, AV continues to embed safety, excellence and compassion in every response.
Best Care, Everywhere is not just a framework, it is our shared commitment to safe, effective, person-centred, and connected care, today and into the future.
Research publications
- Andrews T, Meadley B, Gabbe B, Beck B, Dicker B, Cameron P. Review article: Pre-hospital trauma guidelines and access to lifesaving interventions in Australia and Aotearoa/New Zealand. Emergency Medicine Australasia. 2024;36(2):197-205.
- Alhenaki A, Alqudah Z, Williams B, Nehme E, Nehme Z. Clinical state transitions in shock-refractory ventricular fibrillation: an observational study. Resuscitation. 2025;211:110618.
- lrawashdeh A, Al-Nusair M, Rawashdeh S, Abdi D, Kheirallah KA, Alqahtani S, Alwidyan M, Oteir A, Raffee L, Nehme Z. Temporal trends in the incidence and outcomes of cardiopulmonary arrest events treated in the emergency department at a tertiary hospital in Jordan. Resuscitation Plus. 2025;22:100907.
- Alrawashdeh A, Alqahtani S, Alkhatib ZI, Kheirallah K, Melhem NY, Alwidyan M, Al-Dekah AM, Alshammari T, Nehme Z. Applications and Performance of Machine Learning Algorithms in Emergency Medical Services: A Scoping Review. Prehosp Disaster Med. 2024 Oct;39(5):368-378.
- Andrews T, Dipnall JF, Gabbe BJ, Beck B, Cox S, Cameron PA. Factors associated with a positive shock index in the pre-hospital setting after major trauma. Scand J Trauma Resusc Emerg Med. 2025:9;33(1):122.
- Armour R, Nielsen S, Buxton JA, Bolster J, Han MX, Ross L. Initiation of buprenorphine in the emergency department or emergency out-of-hospital setting: A mixed-methods systematic review. The American Journal of Emergency Medicine. 2025;88:12-22.
- Arthurson L, Harrison S, Clissold B, Bladin C, Howlett G, Ng F, Choi PMC. Bridging the Urban and Regional Divide in Stroke Care (BUILDS): A Novel Telestroke Unit Service. Australian Journal of Rural Health. 2025;33(3):e70067.
- Baldwin R, Baidawi S, Grove C, Lam T, Ogeil RP, Nehme Z, Faulkner A, Beard N, Lubman DI, Scott D. Differences in ambulance attendances between children with and without an identified history of out-of-home-care. Child Abuse and Neglect. 2024;158:107086.
- Ball J, Mahony E, Nehme E, Voskoboinik A, Hogarty J, Dawson LP, Horrigan M, Kaye DM, Stub D, Nehme Z. The burden of atrial fibrillation on emergency medical services: A population-based cohort study. International Journal of Cardiology. 2024:414;132397.
- Beard N, Wilson J, Rowland BC, Nehme Z, Lubman DI, Ogeil RP. Patterns of Acute Gamma-Hydroxybutyrate Harms Requiring Ambulance Attendance: Should Greater Focus Be on Regional Areas? Drug and Alcohol Review. 2025.
- Bloom JE, Goel V, Anderson D, Cartledge S, Nehme Z, Ball J, Eliakundu A, Chan W, Chew DP, Kaye DM, Stub D. Current Emergency Medical Service Vasoactive Use for the Management of Shock. Critical Care Explorations. 2024;6(12).
- Boulton AJ, Abelairas-Gómez C, Olaussen A, Skrifvars MB, Greif R, Yeung J. Cardiac arrest centres for patients with non-traumatic cardiac arrest: A systematic review. Resuscitation. 2024;203.
- Bourke EM, Douglas N, Nehme Z, Knott J, Craig SS, Babl FE. Qualitative Exploration of Health Care Professionals’ Experiences Caring for Young People With Acute Severe Behavioral Disturbance in the Acute Care Setting. Journal of the American College of Emergency Physicians Open. 2025;6(1):100030.
- Broadbear JH, Ogeil RP, McGrath M, Scott DS, Nehme Z, Moayeri F, Lubman D, Rao S. Ambulance attendances involving personality disorder – investigation of crisis-driven re-attendances for mental health, alcohol and other drug, and suicide-related events. Journal of Affective Disorders Reports. 2025;20:100882.
- Cadilhac DA, Birhanu MM, Churilov L, Zhao H, Coote S, Campbell BCV, Langenberg F, Davis SM, Donnan GA, Smith K, Kim J. Costs and Benefits of the Melbourne Mobile Stroke Unit Compared With Standard Ambulance: Causal Analysis Using Observational Linked Data. Stroke. 2025;56(4):948-956.
- Cortegiani A, Ippolito M, Abelairas-Gómez C, Nabecker S, Olaussen A, Lauridsen KG, Lin Y, Sawyer T, Yeung J, Lockey AS, Cheng A, Greif R. In situ simulation for cardiopulmonary resuscitation training: A systematic review. Resuscitation Plus. 2025;21.
- Coull J, Riley B, Anderson D, Richardson S. ECPR in the Emergency Department. Emergency Medicine Australasia. 2025;37(3).
- Cudini D, Smith K, Shao J, Bernard S, Okyere D, Nehme Z, Nehme E, Anderson D, Magnuson N, Thursky K, Mori D, Oosthuizen DW, Udy A. Blood culture collection and administration of intravenous ceftriaxone by paramedics in patients with suspected sepsis (the pass trial). Emergency Medicine Australasia. 2025;37(2):e70027.
- Dawson LP, Ball J, Wilson A, Emerson L, Voskoboinik A, Nehme Z, Horrigan M, Kaye D, Kalman JM, Kistler PM, Stub D. Health Care Cost Burden of Atrial Fibrillation Presentations to Emergency Departments. JACC: Clinical Electrophysiology. 2025;11(6):1342-1344.
- Dawson LP, Ball J, Wilson A, Emerson L, Voskoboinik A, Nehme Z, Horrigan M, Kaye D, Stub D. Association between temperature and air pollutants with atrial fibrillation presentations to emergency departments. Journal of Cardiovascular Electrophysiology. 2025;36(1):71-80.
- Delardes B, Gooley M, Bowles K-A, Chakraborty S. Paramedic to general practitioner referral pathways within Australian jurisdictional ambulance clinical practice guidelines: a document analysis. Australian Health Review. 2025;49(2).
- Delardes B, Gregers MCT, Nehme E, Ray M, Hall D, Walker T, Anderson D, Okyere D, Dantanarayana A, Nehme Z. Smartphone-activated volunteer responders and survival to discharge after out-of-hospital cardiac arrests in Victoria, 2018–23: an observational cohort study. Medical Journal of Australia. 2025;222(10):504-509.
- Delardes B, Powell M, Bowles KA, Chakraborty S, Smith K, Olaussen A. Paramedic perceptions of conveying patients to an emergency department who were suitable for primary care: a cross-sectional survey. Australian Journal of Primary Health. 2024;30(5).
- Delardes BJ, Nehme Z, Bowles K-A, Chakraborty S, Mahony E, Smith K, Talevski J, Sher L, Nehme E. Trends in paramedic-to-general practitioner referrals following the COVID-19 pandemic and the introduction of a virtual emergency department: an interrupted time series analysis. Emergency Medicine Journal. 2025;42(7):460.
- Dwivedi DB, Ball J, Smith K, Nehme Z. Incidence and outcomes of out-of-hospital cardiac arrest from initial asystole: a systematic review and meta-analysis. Resuscitation. 2025;212.
- Eastwood K, Batt A, Tavares W. The importance of outcome measures that matter in paramedicine research. Paramedicine. 2025;22(1):1-5.
- Eastwood KJ, Shi A, Howell S, Buttery A, Bray JE. Sex differences in the intention and decision to use emergency medical services for acute coronary syndrome in Australia: a retrospective study. Emergency Medicine Journal. 2025;42(2):108-116.
- Eliakundu AL, Bloom JE, Ball J, Nehme E, Okyere D, Heritier S, Voskoboinik A, Dawson L, Cox S, Anderson D, Burrell A, Pilcher D, Chew DP, Kaye D, Nehme Z, Stub D. Pre-hospital factors predicting mortality in patients with shock: state-wide linkage study. Open Heart. 2024;11(2):e002799.
- Eliakundu AL, Kim J, Smith K, Kilkenny MF, Birhanu MM, Bagot KL, Nehme E, Cox S, Campbell BCV, Clissold B, Dewey HM, Rabaut J, Ma H, Bladin CF, Cadilhac DA. Adherence to ambulance performance indicators and patient outcomes after stroke: An Australian data linkage study. Australas Emerg Care. 2025:4:S2588-994X(25)00031-4.
- Fisher K, Rice SM, Scott D, Lubman DI, Oliffe JL, Ogeil RP, Beard N, Nehme Z, Seidler ZE. Young men’s anxiety presentations to Australian ambulance services. Journal of Affective Disorders. 2025;384:98-106.
- Gooley M, Delardes B, Hopkins S, Oswald J, Cameron C, Nehme E. Palliative paramedicine: An interrupted time series analysis of pre-hospital guideline efficacy. Palliative Medicine. 2025;39(6).
- Grasner J-T, Bray JE, Nolan JP, Iwami T, Ong MEH, Finn J, McNally B, Nehme Z, Sasson C, Tijssen J, Lim SL, Tjelmeland I, Wnent J, Dicker B, Nishiyama C, Doherty Z, Welsford M, Perkins GD. Cardiac arrest and cardiopulmonary resuscitation outcome reports: 2024 update of the Utstein Out-of-Hospital Cardiac Arrest Registry template. Resuscitation. 2024;201.
- Greif R, E. Bray J, Djärv T, R. Drennan I, G. Liley H, Ng K-C, Cheng A, J. Douma M, R. Scholefield B, Smyth M, Weiner G, Abelairas-Gómez C, Acworth J, Anderson N, L. Atkins D, C. Berry D, Bhanji F, W. Böttiger B, N. Bradley R, Breckwoldt J, N. Carlson J, Cassan P, Chang W-T, P. Charlton N, Phil Chung S, Considine J, Cortegiani A, T. Costa-Nobre D, Couper K, Bittencourt Couto T, N. Dainty K, Dassanayake V, G. Davis P, A. Dawson J, R. de Caen A, D. Deakin C, Debaty G, del Castillo J, Dewan M, Dicker B, Djakow J, J. Donoghue A, Eastwood K, El-Naggar W, Escalante-Kanashiro R, Fabres J, Farquharson B, Fawke J, Fernanda de Almeida M, M. Fernando S, Finan E, Finn J, E. Flores G, E. Foglia E, Folke F, A. Goolsby C, Granfeldt A, Guerguerian A-M, Guinsburg R, Malta Hansen C, Hatanaka T, G. Hirsch K, J. Holmberg M, Hooper S, V. Hoover A, Hsieh M-J, Ikeyama T, Isayama T, J. Johnson N, Josephsen J, Katheria A, D. Kawakami M, Kleinman M, Kloeck D, Ko Y-C, Kudenchuk P, Kule A, Kurosawa H, Laermans J, Lagina A, G. Lauridsen K, J. Lavonas E, C. Lee H, Han Lim S, Lin Y, S. Lockey A, Lopez-Herce J, Lukas G, Macneil F, K. Maconochie I, Madar J, Martinez-Mejas A, Masterson S, Matsuyama T, Mausling R, J.D. McKinlay C, Meyran D, Montgomery W, T. Morley P, J. Morrison L, L. Moskowitz A, Myburgh M, Nabecker S, Nadkarni V, Nakwa F, J. Nation K, Nehme Z, Nemeth M, Nicholson T, Nikolaou N, Nishiyama C, Norii T, Nuthall G, Ohshimo S, Olasveengen T, Olaussen A, Ong G, Orkin A, J. Parr M, D. Perkins G, Pocock H, Rabi Y, Raffay V, Raitt J, Raymond T, Ristagno G, Rodriguez-Nunez A, Rossano J, Rüdiger M, Sandroni C, L. Sawyer T, M. Schexnayder S, Schmölzer G, Schnaubelt S, Lene Seidler A, Semeraro F, M. Singletary E, B. Skrifvars M, M. Smith C, Soar J, Lee Solevåg A, Soll R, Stassen W, Sugiura T, Thilakasiri K, Tijssen J, Kumar Tiwari L, Topjian A, Trevisanuto D, Vaillancourt C, Welsford M, H. Wyckoff M, Yang C-W, Yeung J, M. Zelop C, A. Zideman D, P. Nolan J, M. Berg K. 2024 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations: Summary From the Basic Life Support; Advanced Life Support; Pediatric Life Support; Neonatal Life Support; Education, Implementation, and Teams; and First Aid Task Forces. Resuscitation. 2024;205.
- Haji K, Vogrin S, D’Elia N, Noaman S, Bloom JE, Lefkovits J, Reid C, Brennan A, Dinh DT, Nicholls S, Nehme E, Nehme Z, Smith K, Stub D, Ball J, Zaman S, Oqueli E, Kaye D, Cox N, Chan W. Effect of COVID-19 Pandemic Lockdown on Emergency Medical Service Utilisation, and Percutaneous Coronary Intervention Volume-An Australian Perspective. Heart Lung and Circulation. 2024;33(8):1151-1162.
- Han MX, Ross L, Hemingway L, Anderson D, Gosling C. Out-of-hospital paramedic interactions with people living with dementia: a scoping review. Age and Ageing. 2024;53(7).
- Harris R, Drummond SPA, Meadley B, Rajaratnam SMW, Williams B, Smith K, Bowles KA, Nguyen E, Dobbie ML, Wolkow AP. Adaptive sleep behaviours and shift work tolerance during the transition to shift work. Sleep Medicine. 2024;124:483-93.
- Hartley R, Nehme Z, Schultz B, Nehme E. Out-of-hospital neck of femur injury: An eight-year observational analysis. Pre-hospital Emergency Care. 2025.
- Hew A, Young JT, Rowland B, Scott D, Nehme Z, Arunogiri S, Lubman DI. Exploring the reliability and profile of frequent mental health presentations using different methods: An observational study using statewide ambulance data over a 4-year period. Australian & New Zealand Journal of Psychiatry. 2025;59(1):74-85.
- Howell S, Nehme Z, Ball S, Doan T, Finn J, Bosley E, Faddy S, Dicker B, Swain A, Cameron P, et al. The impact of the COVID-19 pandemic on resuscitation attempts, bystander CPR and survival outcomes in Australia and New Zealand: A binational population-based, Epistry study. Resuscitation Plus. 2025;22:100894.
- Humar M, Meadley B, Cresswell B, Nehme E, Groombridge C, Anderson D, Nehme Z. Cricothyroidotomy in out-of-hospital cardiac arrest: An observational study. Resuscitation Plus. 2024;20:100833.
- Humar M, Meadley B, Groombridge C, Cresswell B, Anderson D, Nehme Z. Bag-valve-mask resuscitators fitted with pressure-limiting valves – Safety feature or potential hazard? Resuscitation Plus. 2024;20:100789.
- John-White MR, Proper E, Muscara F, Babl FE, Anderson VA, Wilson CL, Borland ML, Tonge BJ, Gray KM, Melvin GA, Kochar A, Borschmann R, Haslam R, Tavender EJ, Gordon MS, Dalziel SR, Smith K, Craig SS. Research themes and key data points for child and adolescent emergency department mental health presentations: A national Delphi study. Academic Emergency Medicine. 2025;32(5):542-552.
- Kennedy C, Nehme E, Anderson D, Dantanarayana A, Delardes B, Nehme Z. Changes in out-of-hospital cardiac arrest resuscitation quality during and after the COVID-19 pandemic. Resuscitation. 2024:110419.
- Kleinig TJ, McMullan P, Cloud GC, Bladin PC, Ranta A. Hyper-Acute Stroke Systems of Care and Workflow. Current Neurology and Neuroscience Reports. 2024;24(10):495-505.
- La Gerche A, Paratz ED, Bray JE, Jennings G, Page G, Timbs S, Vandenberg JI, Abhayaratna W, Chow CK, Dennis M, Figtree GA, Kovacic JC, Maris J, Nehme Z, Parsons S, Pflaumer A, Puranik R, Stub D, Freitas E, Zecchin R, Cartledge S, Haskins B, Ingles J. A Call to Action to Improve Cardiac Arrest Outcomes: A Report From the National Summit for Cardiac Arrest. Heart Lung and Circulation. 2024;33(11):1507-1522.
- Lane TJ, Smith CL, Gao CX, Ikin JF, Xu R, Carroll MTC, Nehme E, Abramson MJ, Guo Y. Long-term effects of a coalmine fire on hospital and ambulance use: An interrupted time series study. Environmental Research. 2024;261:119693.
- Lawrence D, Rikkers W, Bartlett J, Barrett S, Seth R, Van Hooff M, Lawn S. Development of the post-traumatic stress disorder assessment scale for emergency services. Arch Environ Occup Health. 2024;79(7-8):235-246.
- Le PH, Cox S, Delir Haghighi P, Wybrow M, Smith K, Nehme Z. Utilization of Emergency Medical Services by Culturally and Linguistically Diverse Patients: A Population-Based Retrospective Study. Pre-hospital Emergency Care. 2024;28(8):988-997
- Lindsay HL, Humar MJ, Anderson DJ, Meadley BN. Optimizing Preoxygenation for Pre-hospital Emergency Anesthesia and Air Medical Transport: A Comparative Study of Bag Refill Valve and Reservoir Bag. Air Medical Journal. 2025;44(4):286-290.
- Maria S, Colbeck M, Wilkinson-Stokes M, Moon A, Thomson M, Ballard J, Parker L, Watson F, Oswald J. Paramedic clinical practice guideline development in Australia and New Zealand: A qualitative descriptive analysis. Australasian Emergency Care. 2024;27(4):259-267.
- Masterson S, Norii T, Yabuki M, Ikeyama T, Nehme Z, Bray J. Real-time feedback for CPR quality – A scoping review. Resuscitation Plus. 2024;19:100730.
- Meadley BN, Caldwell-Odgers J. A comparison of historical versus proposed physical employment standards for flight paramedics performing helicopter winch rescue. Work. 2024;79(3):1333-1341.
- Mitra B, Bernard S, Yankoff C, Somesh A, Stewart C, Koolstra C, Talarico C, Nehme Z, Fitzgerald MC, Cameron PA. Change from semi-rigid to soft collars for pre-hospital management of trauma patients: An observational study. Journal of the American College of Emergency Physicians Open. 2024;5(4):e13239.
- Mitra B, Essery M, Somesh A, Talarico C, Olaussen A, Anderson D, Meadley B. Agreement of point-of-care and laboratory lactate levels among trauma patients and association with transfusion. Vox Sanguinis. 2025;120(2):188-192.
- Mnatzaganian G, Giallo R, Martin R, Crombie A, Nehme Z, Delardes B, Burns D, Furness S, Lenten T, Sharples R, Hanson L, Huxley R. Trends in the complexity of self-harm hospitalisations over 11 years at a major regional hospital in Victoria, Australia: a retrospective study. Frontiers in Psychiatry. 2025;16.
- Mulvihill C, Muir C, Newstead S, Jaske R, Salmon P. To what extent has a systems thinking approach been applied to understand motor vehicle crashes involving ambulances? A systematic review of risk factors and characteristics. Safety Science. 2025;184.
- Nanjayya VB, Fulcher B, Nehme E, Neto AS, Nichol A, Kaye DM, James Cooper D, Nehme Z, Bernard S, Pellegrino V, Higgins AM, Hodgson CL. Long-term health-related quality of life in survivors of extracorporeal cardiopulmonary resuscitation compared to conventional cardiopulmonary resuscitation- A cohort study using Australian and New Zealand extracorporeal membrane oxygenation registry and the Victorian Ambulance Cardiac Arrest Registry. Resuscitation. 2025;210:110601.
- Nehme E, Anderson D, Salathiel R, Carlyon A, Stub D, Cameron PA, Wilson A, Smith S, McNeil JJ, Nehme Z. Out-of-hospital cardiac arrests in Victoria, 2003-2022: retrospective analysis of Victorian Ambulance Cardiac Arrest Registry data. Medical Journal of Australia. 2024;221(11):603-611.
- Nørskov AS, Considine J, Nehme Z, Olasveengen TM, Morrison LJ, Morley P, Bray JE. Removal of bra for pad placement and defibrillation – A scoping review. Resuscitation Plus. 2025;22:100885.
- O’Leary KM, Henderson R, Odgers JNC, Meadley BN. Maintenance of normothermia in the out-of-hospital setting: A pilot comparative crossover study of a foil blanket versus self-warming blanket. Australasian Emergency Care. 2025;28(2):116-122.
- Ogeil RP, McGrath M, Grigg J, Peart A, Meddings JI, Greenwood CJ, Nehme Z, Lubman DI. Diverging trends in alcohol-related harms: The role of comorbid mental health, suicide and self-harm behaviors in ambulance attendances for alcohol intoxication during the COVID-19 pandemic in Victoria, Australia. Journal of Affective Disorders. 2025;371:170-6.
- Orman Z, Olaiya MT, Thrift AG, Cadilhac DA, Phan T, Nelson MR, Ung D, Srikanth VK, Bladin CF, Gerraty RP, Phillipos J, Kim J. Cost-Effectiveness of an Individualised Management Program after Stroke: A Trial-Based Economic Evaluation. Neuroepidemiology. 2024;58(3):156-165.
- Paratz ED, Nadel J, Humphries J, Rowe S, Fahy L, La Gerche A, Prior D, Celermajer D, Strange G, Playford D. The aortic paradox: a nationwide analysis of 523 994 individual echocardiograms exploring fatal aortic dissection. European Heart Journal Cardiovascular Imaging. 2024;25(10):1423-31.
- Paratz ED, Nehme E, Dantanarayana A, Freedman K, Coakley D, Fahy L, Rowe S, Wilkie B, Trytell A, Anderson D, Pflaumer A, Stub D, La Gerche A, Nehme Z. Cardiac arrest in the Australian Alps: A 20-year analysis. Heart Rhythm O2. 2025;6(6):835-842.
- Park A, Armour R, Cantwell K. Clinical presentation of tension pneumothorax among patients undergoing pre-hospital thoracostomy: A retrospective cohort study. Australas Emerg Care. 2025:S2588-994X(25)00044-2.
- Perona M, Cooklin A, Thorpe C, O’Meara P, Rahman MA. Symptomology, Outcomes and Risk Factors of Acute Coronary Syndrome Presentations without Cardiac Chest Pain: A Scoping Review. European Cardiology Review 2024;19:e12.
- Phan TG, Srikanth VK, Cadilhac DA, Nelson M, Kim J, Olaiya MT, Fitzgerald SM, Bladin C, Gerraty R, Ma H, Thrift AG. Framingham Risk Score Prediction at 12 Months in the STANDFIRM Randomized Control Trial. Journal of the American Heart Association. 2025;14(10):e040254.
- Phillips N, Eapen N, Wilson CL, Nehme Z, Babl FE. Pre-hospital use of spinal precautions by emergency medical services in children and adolescents. Emergency Medicine Australasia. 2025;37(1).
- Pilcher D, Hensman T, Bihari S, Bailey M, McClure J, Nicholls M, Chavan S, Secombe P, Rosenow M, Huckson S, Litton E. The authors reply. Critical Care Medicine. 2025:52(7):p e413-e415.
- Shahab J, Noonan M, Cox S, Nehme Z, Shepherd M, Meadley B, Mitra B, Olaussen A. The diagnostic utility of pre-hospital hyperglycaemia in major trauma patients: An observational study. Emergency Medicine Australasia. 2025;37(1):e14521.
- Sharp S, Tracy L, Singer Y, Schnekenburger M, Burrell A, Paton A, Salerno S, Holden D. Early Acute Kidney Injury in Adult Patients With Burns in Australia & New Zealand. Journal of Surgical Research. 2024;303:482-488.
- Silva W, Fisk B, Caldwell-Odgers JN, Meadley BN. A Comparative Evaluation of Selection Processes for Helicopter Emergency Medical Service Paramedics in Australasia. Air Medical Journal. 2025;44(1):60-66.
- Smith A, Mason R, Kilsby J, Dantanarayana A, Walker T, Nehme Z. Out-of-hospital cardiac arrest secondary to electrocution: Characteristics and outcomes. Resuscitation. 2025.
- Stub D, Batchelor R, Ball J. Double or nothing: Alternative defibrillation strategies reduces downtime in ventricular fibrillation. Resuscitation. 2025;209.
- Stub D, Batchelor RJ, Bloom JE, Kaye DM. Riding the Impella Wave in Cardiogenic Shock: Is it Time for Australia to Get on Board? Heart Lung Circ. 2025;34(7):662-664.
- Yogendrakumar V, Balabanski AH, Johns H, Churilov L, Parsons NK, Beharry J, Weir L, Yassi N, Zhao H, Warwick A, Coote S, Langenberg F, Branagan L, Siddiqi W, Bivard A, Campbell BCV, Donnan GA, Davis SM. Evaluating the Safety and Efficacy of Telemedicine Physician Assessments on a Mobile Stroke Unit: Protocol for a Prospective Open-Label Blinded End-Point Randomized Controlled Trial. Journal of the American Heart Association. 2024;13(21):e036856.
Right care, right patient, right time
We continue to work with our partners to find new and innovative ways of improving patient care, ensuring that our patients are receiving the most appropriate care for their needs and saving ambulances for emergencies.
Over the past year we have continued to develop and expand alternate service pathways and leveraged technology to strengthen our triage capabilities.
Our Patient Management Team has made significant progress in supporting patients with frequent and complex healthcare needs while reducing strain on emergency ambulance resources.
Our work towards improving the experience of patients with mental health conditions as part of Victoria’s mental health reform program is another example of our commitment to delivering the right care to the right patient at the right time.
Video Assisted Triage
The initial success of Video Assisted Triage (VAT) has continued to grow, and the technology is now available to all Triage Practitioners across all our Secondary Triage workstations. The last year also saw the service roll out to our mental health nurses within Triage Services.
With greater visibility of our patients using VAT, we can ensure better accuracy of health outcomes, including recommending whether the patient needs to attend an emergency department.
During 2024, VAT was a finalist in both the Council of Ambulance Authorities Awards of Excellence and the Victorian Public Healthcare Awards.
Key statistics
A total of 35,092 cases managed by Triage Services utilised VAT, and 22,122 (63%) were diverted from emergency ambulance resources and referred to alternate services.
Victorian Virtual Emergency Department
As part of providing the best patient care, AV’s paramedics and triage practitioners can safely connect patients to care options, other than emergency ambulance services, that best meet their health care needs.
The Victorian Virtual Emergency Department (VVED) is one of AV’s most utilised medical telehealth services, offering patients real-time virtual consultations with emergency doctors, where they receive clinical assessments, medical advice, treatment, and appropriate referrals to services such as GPs or residential in-reach teams.
The last 12 months have also seen the service expand to offer specialist services rooms and follow-up calls to ensure continuity of care for users from the comfort of their own homes.
The expansion of VVED services, available at no cost to all Victorians via the VVED website, has continued to improve access to emergency care and alleviate the pressure on ambulance services.
Mental health reform
AV is a partner agency in delivering the Royal Commission into Victoria’s Mental Health System’s Recommendation 10, which aims to achieve a health-led response for people experiencing mental health crises.
AV has supported DH’s development of service design models and frameworks to guide progression of reform activities in 2024-25.
A Service Design Workshop series has informed system and service model design for telehealth models, health-led co-response to mental health emergencies, safe spaces and stabilisation facilities as well as opportunities for diversion of calls from police call takers to ambulance call takers.
Mental health care continues to be a major part of day-to-day work for paramedics. AV continues to engage with the DH legislation team and has completed all amendments in relation to DH/AV operational protocols. These will be finalised once there is alignment with DH and Victoria Police protocols.
Mental health emergencies
Mental health is now AV’s most frequent call type (11%), having overtaken chest pain (10%) and breathing problems (10%).
Last year, AV received 67,380 mental health calls requiring an ambulance dispatch or telephone support via Secondary Triage and a mental health clinician.
Patient Management Team
Our Patient Management Team is dedicated to supporting patients with frequent and complex healthcare needs to receive care that is tailored to their unique social and health needs.
Our team works with these patients to develop personalised patient management plans and mental health information plans, helping them to make informed decisions and link patients with appropriate care.
In 2024-25, the team created 133 new patient management and mental health information plans and reviewed 127 existing plans for tailored support and care coordination.
As a flow-on effect to implementing these plans, strain on our emergency ambulance resources is reduced, and there is a reduced risk of vicarious trauma experienced by community members assisting the patient in a perceived emergency.
Our data provides a compelling case to continue to expand our focus on patient management plans to frequent callers, members in our community who call AV more than 10 times over a three-month period. The top two per cent of frequent callers utilise 14 per cent of total emergency ambulance services. Frequent callers have also increased by 64 per cent over the past five years. This may be attributed to the 24/7 availability of ambulance services, while other services can have limited hours.
However, by identifying and treating the underlying cause of a patient’s presentations, we are able to achieve an average 74 per cent reduction in presentations in four out of five patients. These results have had a significant impact on improving patient care and ambulance availability.
Impact of patient management plans
Patient
- Increase in support services
- Reduced harm from excessive medication
- Reduced carer fatigue
- Better engagement with community supports
- Collaborative care team
AV Staff
- Supported in their clinical decision making
- Reduced occupational violence
- Reduced vexatious claims of abuse
Community
- Improved resourcing
- Reduced bystander exposure
Frequent and complex patients
The top 2% of presenters accounted for 14% of total ambulance workload.
Patients with more than 10 presentations over 3 months has increased by 64% over the past 5 years.
6 months post plan saw 74% reduction in presentations in 4 out 5 patients.
Digital connection and advancements
Our commitment to innovation and connectivity is transforming how we deliver care, making our operations more agile and our patient interactions more seamless. By adopting the latest technologies and enhancing our communication networks, we are empowering our people with the tools they need to respond swiftly and effectively.
Digital Radio Upgrade Program
In 2024-25 the Digital Radio Upgrade Program (DRUP2) for rural areas commenced implementation.
DRUP2 involves the replacement of the RAVNet (analogue) radio network with the Regional Mobile Radio (RMR) digital network, enabling seamless connectivity between the metropolitan digital network and delivering a secure statewide digital radio network for AV.
Online training has prepared AV’s operational workforce for the changes. A dedicated fleet facility was also established in Ballarat to upgrade vehicles with new digital radio equipment, supported by a small team managing logistics to deliver upgraded vehicles and new radios across the state.
Following a soft launch in December 2024, the phased rollout began in January 2025 in Barwon South West, progressing clockwise across the state. To date, just over 50 per cent of the rollout is complete and we are on track to complete the roll-out by mid 2026.
Standardised two-way radio communication systems known as Fixed Station Terminals (FSTs) commenced implementation across 19 Victorian EDs. The primary objective of FSTs is to enhance communication reliability and efficiency for emergency healthcare delivery. Key benefits include direct paramedic-to-ED communication via radio, as well as early notification of high-acuity patient arrivals.
Branch Wi-Fi rollout has occurred at all AV branches enabling portable radios to roam onto AV Wi-Fi to ensure in-branch coverage is maintained at all times.
This, combined with the newly introduced SelCall alerting feature, benefits response by ensuring responders are always audibly notified at the time of case dispatch, even when at their branch. Non-Emergency Patient Transport (NEPT) contractors have received training and delivery of new portable radios. Roll-out commenced for some contractors (St John Ambulance) in July 2025.
Key statistics
Teams across Barwon South West, Grampians and Loddon Mallee regions have received their digital portable and vehicle radios. Hume will commence rollout on 15 July 2025.
- 2,454 staff and volunteers have completed their online training.
- 1291 portable radios have been distributed to rural branches, with 932 now in use. In addition, 139 rural branches have had Wi-Fi activated to enable in-branch radio coverage and connection.
- 10 hospitals across Barwon South West, Grampians and Loddon have received their new FSTs.
- Six additional branch equipment lockers were installed at Torquay, Echuca, Swan Hill, Wonthaggi, and Sale. In total there are now 16 rural lockers across the state that to provide access to spare portable radios.
- 344 vehicles were upgraded to digital radio by the end of June 2025.
- Nine briefcase mobile radios have been deployed for events and natural disaster management.
Mobile Data Network into Rural
Mobile Data Network (MDN) into Rural (MDNR) is a multi-year project, complementing DRUP2. Project funding is approximately $23 million across AV and Emergency Management Victoria (Department of Justice and Community Safety).
Since 2006, the metropolitan region has had MDN with Mobile Data Terminal devices (MDTs) fitted into the dash of vehicles to support operational teams with improved situational awareness, two-way data communications (to/from ambulances), navigation to a case and providing encrypted text-based information about the case and patient.
With changes in technology and advances in our fleet, the best option to introduce improved capability such as MDN is to utilise a smartphone and application, leveraging the vehicle’s entertainment system and screen. The first phase of the project is to provide cradles for safe phone use in vehicles and project support to progress the design and planning for implementation.
Installation of cradles is planned to commence by the second half of 2025, following completion of vehicle safety testing. In June 2025 a contract variation was agreed with Motorola, the current MDN supplier, to develop the MDN application for AV Rural. Implementation is planned for the second half of 2026.
VACIS Modernisation (iPad) Project
This year marked the successful completion of the VACIS Modernisation Project, a major digital uplift that involved:
- Replacement of ageing operational laptops with over 5,000 modern, lightweight iPads, setting the foundation for faster and more reliable access to digital tools in the field.
- Significant redesign of the VACIS platform – the core application used by paramedics on their new iPads to complete and submit their patient care records.
The VACIS redesign included a new interface specifically for iPad use, providing a cleaner, faster and more user-friendly experience, and was shaped by our paramedics during extensive in-field testing prior to the roll-out.
As a result of this deep involvement by our operational crews, the rollout model was adjusted to better support the distribution of iPads across the state, ensuring smoother deployment and improved user experience.
Key statistics
57,840 gigabytes of iPad data uploaded since roll-out
Over 5,000 iPads delivered across 83 branches
Deployment of 26 smart lockers – for safe storage of devices and management of repair/replacement
What our workforce is saying
Speech-to-text is a game changer, I can document significantly more, significantly more quickly.
Easy and fast to log in and stay logged in, fast and responsive.
Much quicker start up, halved my VACIS case sheet time to complete.
Our community
We are committed to providing fair access to ambulance and healthcare services, to building healthy and resilient communities, and to continuously improve our service in partnership with Victorians.
We continue to provide engagement and education programs across metropolitan and regional areas in Victoria that build community resilience and improve health outcomes for everyone.
Community and Consumer Engagement Plan progress
The AV’s Community and Consumer Engagement Plan 2023–2028 (CCEP) continues to guide our strategic approach to community engagement.
Anchored in the ‘Patient’ and ‘Connection’ pillars of our Strategic Plan 2023-2028, the CCEP outlines clear goals and measurable outcomes that reflect our commitment to partnering with communities and consumers.
The plan aims to improve access to ambulance and healthcare services, foster resilient communities, and drive continuous service improvement in collaboration with Victorians.
In the second year of delivering the CCEP, we strengthened our connection with the Victorian community through targeted health education initiatives led by paramedics and volunteers.
These initiatives reached over 146,909 individuals, focusing on enhancing public understanding of health emergencies, appropriate use of Triple Zero (000), and alternative care pathways within the health system when an emergency ambulance is not required.
Throughout 2024-25, AV delivered 2,686 community engagement sessions reaching 146,909 people. These included:
- 479 sessions to 29,459 participants, with the aim of building awareness of non-emergency healthcare options. These sessions empowered people to make informed decisions about accessing appropriate care, supporting the sustainability of emergency ambulance services.
- 95 community events with Aboriginal and Torres Strait Islander communities including National Reconciliation Week and NAIDOC Week. These engagements reaffirm AV’s dedication to reconciliation and respectful partnerships.
- Eight LGBTQIA+ and Pride events across Victoria. These included prominent celebrations such as Midsumma Carnival Day, Daylesford ChillOut Festival, South Gippsland Pride, and Bendigo Pride in the Park.
- 159 events and presentations with multicultural communities reaching 6,709 people.
- 736 regional and rural community events and engagements reaching 48,623 people in some of the most remote areas of the state.
Through these events, we reinforced our commitment to fostering inclusive environments and building trust with diverse communities.
Community Forum Series
AV recognises the challenges of distance and access to healthcare that regional and rural communities experience. We understand their needs are unique, and we know that increasing engagement with regional communities is critical to helping us to better meet their needs.
To support this, we commenced a community forum series.
The first forum was facilitated in May 2025 at the Traralgon Golf Club and was an overwhelming success. With 86 participants in attendance, the forum offered a welcoming space for all community members to hear about AV’s strategic direction, share their lived experiences and contribute to shaping the future of ambulance care in Gippsland.
Attendees embraced the opportunity to take part in the world café conversions with members of the Executive Team, Community Advisory Committee and local paramedics, followed by a networking lunch and exhibition including CPR demonstration.
Key themes emerging from the discussions at the forum and the post-event survey include:
- Strengthening trust between AV, its staff, volunteers, and the broader community through transparent communication and responsiveness.
- Enhancing collaboration with local emergency services, health providers, and community groups to improve engagement, education and culturally appropriate care.
- Streamlining coordination between emergency and health services to ensure seamless integration and efficient service delivery.
- Expanding community education on when to call an ambulance and promoting alternative care pathways for non-emergencies.
- Prioritising equity and inclusion to improve access for multicultural communities, First Nations and vulnerable populations.
- Strengthening preparedness and resilience through strategic planning for disasters, ageing populations and infrastructure challenges.
To address these themes, a regional engagement plan is being developed to drive meaningful improvements and AV will continue to partner with community and consumers to inform service design and quality care that is safe, person and family-centred, equitable and clinically effective.
The forum was wonderful! The presentations, with facts were so informative and I loved the world cafe style. The venue and food were also great. I don’t have any suggested improvements; it was really well done. Thank you.
Parents and Carers of Young Children presentation
To help support ambulance resource demand and the needs of our community, we developed a presentation focused on parents and carers of young children. This aims to support parents and carers to access reliable sources of information and make informed decisions on when to call Triple Zero (000) and when to seek alternative pathways if the issue is not an emergency.
AV has partnered with local government Maternal and Child Health Service teams to help deliver this critical information in their local communities, particularly via new parents’ groups.
The presentation highlights:
- When to call Triple Zero (000) and what to expect.
- Where to find reliable sources of information about children’s health, such as Maternal and Child Health Services and The Royal Children’s Hospital fact sheets.
- Alternative healthcare pathways to manage non-urgent care at home, such as the VVED and Urgent Care Clinics.
- Common medical conditions in children and how to address them.
This presentation has been well received by local government maternal health teams and the new parents’ groups they support. In 2024-25, 223 presentations were delivered to 3,423 participants.
Neuroinclusion Toolkit – AV’s Disability Inclusion Program
AV launched its Neuroinclusion Toolkit, developed in collaboration with Australian Disability Network and Amaze, leaders in creating disability inclusive workplaces.
The Toolkit is designed to build understanding and create conversations to better support neurodivergent colleagues and deliver best care in our community.
The toolkit features tailored resources designed in collaboration with people with lived experience, and has inspired many people at AV to complete the accompanying neuroinclusion training.
Resources on the sensory experience of an ambulance, available on AV’s website, have also been warmly welcomed by the community.
Here’s what our people are saying
A neuroinclusive approach values and supports diverse ways of thinking, communicating, and working. Embedding inclusive practices in the workplace has been shown to improve staff wellbeing, retention, innovation, and overall productivity.
Being able to ask questions and make those adjustments to allow people to feel comfortable… enough to be able to answer our questions and allow us to assess them is such a key point.
Play your part, be summer smart campaign
Summer is a welcome time of year for many Victorians, but the warmer months also bring some additional community health risks – including heat-related illnesses, summer storms and the risk of thunderstorm asthma and disease-carrying mosquitoes.
There are simple steps we can take to prepare for these challenges and enjoy our summer safely. Over the summer, AV ran a dedicated campaign to bring attention to a number of messages:
- Keep updated on extreme weather warnings in your area and understand how these might impact your health.
- Have an action plan in place and practice what to do if conditions change.
- If an extreme weather event is unfolding follow your plan, and check in on others around you.
Our campaign involved digital, media and face-to-face engagement, building in messages from government and emergency services summer campaign messaging including Survive the Heat, Never Leave Kids in Cars, Right Care Right Place Right Time, Fire Ready, Water Safety and heatwave preparedness.
We delivered over 110 face-to-face engagements, reaching more than 6,100 Victorians with vital safety information.
Workforce data
This workforce information is provided in accordance with the Minister for Finance’s Reporting Direction 29: ‘Workforce data disclosures in the report of operations – public service employees.’
Total employee numbers
Full-Time Equivalent (FTE) Employees 2024-25 (size of the workforce):
| Employee Numbers (FTE) – Annual Report Category | 2024-25 | 2023-24 |
|---|---|---|
| On road Clinical Employees1 | 4897.32 | 4886.9 |
| Operation Support and Managerial Staff2 | 685.14 | 651.1 |
| Other Managerial, Professional and Administrative Employees3 | 613.31 | 628.3 |
| TOTAL | 6195.77 | 6166.3 |
1. On road Clinical Staff – includes but not limited to Paramedics, Team Managers, Patient Transport Officers, Retrieval Registrars, Clinic Transport Officers and Clinical Instructors.
2. Operation Support and Managerial Staff – includes but not limited to Senior Team, Area and Regional Managers, Rosters staff, Communications staff, Rehab Advisors, OHS Advisors, Logistics staff, Fleet staff, Duty Team Managers, Telecommunication staff and Clinical Practice staff.
3. Other Managerial, Professional include all other staff who do not fall into the above two categories.
Ambulance Community Officers
AV employs 894 casual Ambulance Community Support Officers (ACOs) who also provide emergency response alongside our paramedics. These employees are represented in the above on-road clinical employee FTE numbers based on their hours worked converted to equivalent full-time positions.
Community Emergency Response Team volunteers
AV engages 177 Community Emergency Response Team (CERT) volunteers who provided emergency response in 2024-25.
Mobile Intensive Care Ambulance paramedics (MICA)
This group of MICA employees forms part of AV’s Full-Time Equivalent Employees 2024-25:
| MICA Employee Numbers | 2024-25 | 2023-24 |
|---|---|---|
| MICA Full-Time Equivalent Employees | 508.32 | 503.45 |
| MICA Full-Time Equivalent Trainees | 79.78 | 82.9 |
| TOTAL | 588.1 | 586.4 |
Newly recruited paramedics
In 2024-25, AV continued to strengthen its operational workforce through a targeted recruitment strategy. The approved recruitment target for the year was 229 new paramedics, reflecting our commitment to meeting growing service demands and supporting community health across Victoria.
This intake included a diverse mix of entry pathways: 43 GAPs began their careers with AV, while 154 recruits joined through the Medium Acuity Transport Graduate Bridging Program. A further 11 paramedics commenced via the Rural Sponsored Degree Program, helping to bolster services in regional and rural communities.
In addition, 18 qualified paramedics transitioned from interstate ambulance services, bringing valuable experience to the team, and three internal staff moved from casual to permanent roles. Recruitment efforts began in the final months of 2023-24, with 83 paramedics commencing in May and June 2024, contributing to the 2024-25 target. The remaining 146 paramedics were onboarded throughout the year, successfully fulfilling the recruitment goal.
Looking ahead, 60 paramedics commenced with AV in June 2025, forming part of the 2025-26 recruitment target, which stands at 294 as of July 2025. This continued growth reflects our strategic focus on workforce sustainability and readiness to meet future challenges.
Health, safety and wellbeing
Occupational health and safety
Occupational health and safety remain a cornerstone of our commitment to our people. Paramedics face unique physical and psychological challenges that require proactive and comprehensive safety measures. Ensuring strong health and safety practices not only protects our workforce, but it also directly contributes to better patient care and service delivery.
Through our Health and Safety Action Plan, AV continues to address key risks such as fatigue, occupational violence, manual handling, and psychosocial hazards. These targeted strategies are designed to reduce injury and illness, while fostering a culture of resilience, safety, and wellbeing.
By focusing on prevention and early intervention, and by supporting staff when injuries do occur, AV is building a sustainable and engaged workforce, one that is equipped to meet the demands of the role and deliver exceptional care to the Victorian community.
| 2024-25 | 2023-24 | 2022-23 | |
|---|---|---|---|
| Number of workplace fatalities | 0 | 1 | 0 |
| Lost Time Injury Frequency Rate (LTIFR)1 | 102.0 | 96.4 | 77.99 |
| Average number of Standard claims per 100 FTE (Full time Equivalent) employees1 | 10.6 | 10.4 | 10.8 |
| Average number of Standard claims per 1,000,000 hours worked1 | 70.5 | 66.7 | 69.5 |
| Average cost per WorkCover Standard claim2 | $92,097 | $111,806 | $101,120 |
| Number of reported hazards/incidents for the year per 100 FTE3 | 83.8 | 80.2 | 59.5 |
| Percentage of WorkCover Standard claims with a RTW plan initiated4 | 95 | 86 | 100 |
| Percentage of employees immunised against influenza (including ACOs)5 | 79.5 | 91.3 | 88.1 |
| Number of Health and Safety Representatives (HSR) positions filled6 | 356 | 341 | 297 |
Notes
1. An increased number of standard WorkCover claims in 2024-25 impacted the LTIFR, the average number of standard claims per 100 FTE and the average cost per WorkCover standard claim rates. The average number of standard claims per 1,000,000 hours worked is impacted by both an increase in volume of standard claims received, and the fluctuating nature of productive hours worked.
2. Claims costs mature over time, and as such the data captured reflects the costs received as at the end of June 2025. Claims costs from previous financial years will have matured and consequently figures will differ from previous annual reports.
3. The number of hazards / incidents / injuries (HIIs) as logged in AV’s Health Safety and Claims System per 100 FTE.
4. The percentage of Standard claims with return-to-work plans is calculated from a sample and excludes claims with less than 10 days’ time loss. AV’s result of 95 per cent reflects the significant increase in overall claims volume, and the resulting resourcing impact.
5. The percentage of employees immunised is reflective of the final percentage with the 2023-24 influenza season, August 2024.
6. HSRs have increased in number over the past three years and align with the growth in the paramedic workforce and the number of AV locations. Number includes Deputy HSRs.
Definitions
a. Accepted WorkCover claims – accepted WorkCover claims that were lodged in financial year.
b. Lost Time – defined as greater than one day.
Occupational violence
Everyone has a right to a safe working environment.
Occupational violence (OV) poses serious risks to the mental and physical health of our people, as well as job satisfaction and the quality of patient care.
| Occupational violence statistics 2024-25 | |
|---|---|
| WorkCover accepted claims with an occupational violence cause per 100 FTE | 1.0 |
| Number of accepted WorkCover claims with lost time injury with an occupational violence cause per 1,000,000 hours worked | 6.3 |
| Number of Occupational Violence Hazard, Incidents or Injuries (HII’s) reported | 1045 |
| Number of Occupational Violence HII’s reported per 100 FTE | 16.9 |
| Percentage of Occupational Violence HII’s resulting in injury, illness or condition | 5.93% |
Due to the nature of their work, paramedics often operate in uncontrolled environments such as private homes and public spaces, where risks cannot be fully eliminated. AV prioritises management strategies to minimise harm, including the right for AV people to tactically withdraw from unsafe scenes and seek support, such as police assistance, before continuing emergency care.
In 2024-25, OV injuries per million hours worked decreased by five per cent compared to the previous year, demonstrating the effectiveness of targeted safety interventions. Near-miss reporting also increased by 10 per cent, indicating a strengthened reporting culture and proactive risk identification across the organisation.
Other dedicated OV-prevention and preparedness initiatives from the past year include:
- Continuation of our comprehensive risk-based OV prevention program, featuring an overarching framework, annual work plans, and a statewide consultative working group.
- Expansion of training initiatives with paramedic graduates receiving a full day of face-to-face OV training.
- Resources for call takers in our communication centres.
- Roll-out of mandatory OV learning modules, designed to equip our people with practical strategies for managing risk and enhancing personal safety.
Environmental report
Environmental performance
AV is committed to reducing our impact on the environmental footprint. Our Sustainability Action Plan outlines the steps we are taking to play our part in creating a better environment for us all, and our commitment to achieving net zero carbon by 2045 remains strong.
AV’s environmental reporting for 2024-25 is developed in line with Financial Reporting Disclosure requirements (FRD24) from the Victorian Government Department of Treasury and Finance.
Electricity EL1-EL4
Energy efficiency projects such as LED lighting replacement and heat pump water replacement have reduced demand for electricity. The total on site electricity generated continues to increase, in 2024-25 by 1.5 per cent.
Stationary Energy F1-F2
Stationary energy use has reduced across the last three years with 2024-25 resulting in the lowest consumption across the three years. Stationary energy, which consists of natural gas from a pipeline and liquid petroleum gas (LPG), contributes to less than one per cent of AV emissions. AV continues to see an overall reduction in gas usage as a result of an active transition from gas to electric.
Transportation Energy T1-T4*
AV continues to be challenged in reducing fuel usage and the associated emissions from our fleet due to the duty cycle and payload of our vehicles, together with the requirement for specific road vehicles and aircraft platforms. In 2024-25 reduced its transportation energy consumption by 1.2 per cent.
AV is committed to exploring ways that we can transition our fleet away from fossil fuels. A Zero Emission Vehicle Plan is currently being developed to help AV achieve net zero carbon by 2045.
Total energy use E1-E4*
Electricity and transport energy consumption continued to decrease while the renewable energy component continues to increase.
Water use W1-W2
Water use increased slightly in 2024-25. AV continues to use VicFacilities to monitor our water usage. Typically, the bulk of AV’s water is consumed at corporate sites.
Waste and recycling WR1-WR5*
Waste and recycling data that has been reported in 2024-25 is significantly lower than previous years. AV has not been able to conduct audits in 2024-25, however intends to in 2025-26, which could change the reported data in 2024-25 for WR1-WR5.
Greenhouse Gas Emissions G1-G3*
AV continues to maintain a strong focus on emissions reduction. Overall AV have decreased greenhouse gas emissions 0.81 per cent.
The transition of all AV sites on the electricity State Purchasing Contract to 100 per cent GreenPower has continued to stabilise Scope 2 emissions.
Continued high demand on the ambulance service has seen figures relatively consistent with case numbers in 2023-24. The continued high demand in case numbers and decreased emissions demonstrates that we are working to efficiency reduce emissions where we can while we deliver healthcare services.
*In 2024-25, AV recalculated how it collects it transportation energy and has reflected this for 2022-23 and 2023-24. This recalculation is based on a reliable data set. AV also intends to conduct an audit in 2025-26 into waste and recycling to ensure that it is reporting accurately.
Electricity use
EL1 total electricity consumption segmented by source (MWh)
| Apr 24 – Mar 25 | Apr 23 – Mar 24 | Apr 22 – Mar 23 | |
|---|---|---|---|
| Purchased | 7,618.82 | 7,535.80 | 8,078.56 |
| Self-generated | 406.54 | 415.79 | 380.66 |
| EL1 Total electricity consumption (MWh) | 8,025.36 | 7,951.59 | 8,459.22 |
EL2 On site-electricity generated (MWh) segmented by:
| Apr 24 – Mar 25 | Apr 23 – Mar 24 | Apr 22 – Mar 23 | |
|---|---|---|---|
| Consumption behind-the-meter Solar Electricity | 406.49 | 415.79 | 380.66 |
| Total Consumption behind-the-meter (MWh) | 406.49 | 415.79 | 380.66 |
| Exports | |||
| Solar Electricity | 116.98 | 99.90 | 132.66 |
| Total Electricity exported (MWh) | 116.98 | 99.90 | 132.66 |
| EL2 Total On site-electricity generated (MWh) | 523.48 | 515.70 | 513.31 |
EL3 On-site installed generation capacity (kW converted to MW) segmented by:
| Apr 24 – Mar 25 | Apr 23 – Mar 24 | Apr 22 – Mar 23 | |
|---|---|---|---|
| Solar System | 0.48 | 0.45 | 0.45 |
| EL3 Total On-site installed generation capacity (MW) | 0.48 | 0.45 | 0.45 |
EL4 Total electricity offsets segmented by offset type (MWh)
| Apr 24 – Mar 25 | Apr 23 – Mar 24 | Apr 22 – Mar 23 | |
|---|---|---|---|
| GreenPower | 6,992.50 | 6,852.20 | 4,864.28 |
| RPP (Renewable Power Percentage in the grid) | 1,415.35 | 1,412.26 | 1,518.77 |
| EL4 Total electricity offsets (MWh) | 7,618.82 | 7,535.80 | 6,383.05 |
Stationary energy
F1 Total fuels used in buildings and machinery segmented by fuel type (MJ)
| Apr 24 – Mar 25 | Apr 23 – Mar 24 | Apr 22 – Mar 23 | |
|---|---|---|---|
| Natural gas | 1,176,703.55 | 1,359,638.63 | 1,966,742.21 |
| LPG | 39,210.40 | 57,053.70 | 68,853.00 |
| Diesel | 63,331.20 | 76,675.00 | 115,900.30 |
| F1 Total fuels used in buildings (MJ) | 1,279,245.15 | 1,493,367.33 | 2,151,495.51 |
F2 Greenhouse gas emissions from stationary fuel consumption segmented by fuel type (CO2-e(t))
| Apr 24 – Mar 25 | Apr 23 – Mar 24 | Apr 22 – Mar 23 | |
|---|---|---|---|
| Natural gas | 60.64 | 70.06 | 101.35 |
| LPG | 2.38 | 3.46 | 4.17 |
| Diesel | 4.45 | 5.38 | 8.14 |
| F2 Greenhouse gas emissions from stationary fuel consumption (CO2-e(t)) | 67.46 | 78.90 | 113.65 |
Transportation energy
T1 Total energy used in transportation (vehicle fleet) within the Entity, segmented by fuel type (MJ)
| Apr 24 – Mar 25 | Apr 23 – Mar 24 | Apr 22 – Mar 23 | |
|---|---|---|---|
| Non-emergency transport (Health service operated) – Gasoline | 1,566,333.10 | 3,382,595.70 | 4,222,523.50 |
| Non-executive fleet – Gasoline | 22,707,093.50 | 24,512,843.40 | 22,881,855.50 |
| Road ambulance – Gasoline | 4,672,550.90 | 5,274,258.90 | 6,454,118.00 |
| Petrol (total) | 28,945,977.50 | 33,169,698.00 | 33,558,497.00 |
| Non-emergency transport (Health service operated) – Diesel | 9,504,208.10 | 8,842,927.80 | 7,643,070.40 |
| Non-executive fleet – Diesel | 8,263,549.80 | 10,196,147.70 | 13,457,488.60 |
| Road ambulance – Diesel | 156,851,474.60 | 159,492,864.90 | 156,560,044.60 |
| Diesel (total) | 174,619,232.50 | 178,531,940.40 | 177,660,603.60 |
| Air ambulance – fixed wing – Aviation Turbine Fuel | 89,651,795.20 | 89,746,478.40 | 92,896,219.80 |
| Air ambulance – fixed wing – Aviation Turbine | 77,457,744.00 | 73,721,476.80 | 80,228,151.00 |
| Aviation turbine fuel (ATF) (total) | 167,109,539.20 | 163,467,955.20 | 173,124,370.80 |
| Electricity for Road Vehicles from Public or Private Chargers | – | 58.40 | – |
| Electricity for Road Vehicles from Victorian Government Facilities | – | 2,620.10 | – |
| Electricity (Transport Energy) (total) | – | 2,678.50 | – |
| Total energy used in transportation (vehicle fleet) (MJ) (total) | 370,674,749.20 | 375,172,272.10 | 384,343,471.40 |
T2 Number and proportion of vehicles in the organisational boundary segmented by engine/fuel type and vehicle category
| Apr 24 – Mar 25 | Apr 23 – Mar 24 | Apr 22 – Mar 23 | |
|---|---|---|---|
| Road vehicles | 1870 | 1704 | – |
| Two and three-wheeled vehicles | 4 | 5 | – |
| Petrol | 4 | 5 | – |
| Passenger vehicles | 741 | 678 | – |
| Petrol | 427 | 395 | – |
| Diesel | 129 | 148 | – |
| Petrol hybrid | 183 | 130 | – |
| PHEV | 2 | 1 | – |
| NULL | 25 | 3 | – |
| EV | 2 | 1 | – |
| Goods Vehicles | 1098 | 1021 | – |
| Petrol | 24 | 36 | – |
| Diesel | 1074 | 981 | – |
| Hybrid | 0 | 4 | – |
T3 Greenhouse gas emissions from transportation (vehicle fleet) segmented by fuel type (CO2-e(t))
| Apr 24 – Mar 25 | Apr 23 – Mar 24 | Apr 22 – Mar 23 | |
|---|---|---|---|
| Non-emergency transport (Health service operated) – Gasoline | 105.92 | 228.73 | 285.53 |
| Non-executive fleet – Gasoline | 1,535.45 | 1,657.56 | 1,547.27 |
| Road ambulance – Gasoline | 315.96 | 356.65 | 436.43 |
| Petrol | 1,957.33 | 2,242.94 | 2,269.23 |
| Non-emergency transport (Health service operated) – Diesel | 669.19 | 622.85 | 538.91 |
| Non-executive fleet – Diesel | 581.84 | 718.16 | 948.89 |
| Road ambulance – Diesel | 11,043.91 | 11,229.89 | 11,023.39 |
| Diesel | 12,294.94 | 12,570.91 | 12,511.19 |
| Air ambulance – fixed wing – Aviation Turbine Fuel | 6,294.45 | 6,301.10 | 6,522.24 |
| Air ambulance – rotary wing – Aviation Turbine Fuel | 5,438.31 | 5,175.98 | 5,632.82 |
| Aviation turbine fuel (ATF) | 11,732.76 | 11,477.09 | 12,155.06 |
| Electricity for Road Vehicles from Public or Private Chargers | – | 0.01 | – |
| Electricity for Road Vehicles from Victorian Government Facilities | – | 0.48 | – |
| Electricity (Transport Energy) | – | 0.50 | – |
| Total Greenhouse gas emissions from transportation (vehicle fleet) (CO2-e(t)) | 25,985.03 | 26,291.42 | 26,935.48 |
T4 Total distance travelled by commercial air travel (passenger km travelled for business purposes by entity staff on commercial or charter aircraft)
| Apr 24 – Mar 25 | Apr 23 – Mar 24 | Apr 22 – Mar 23 | |
|---|---|---|---|
| Total distance travelled by commercial air travel | 19,304.00 | 85,820.86 | 148,742.01 |
T(opt1) Total vehicle travel associated with entity operations (1,000 km)
| Apr 24 – Mar 25 | Apr 23 – Mar 24 | Apr 22 – Mar 23 | |
|---|---|---|---|
| Total vehicle travel associated with entity operations (1,000 km) | 42,922.94 | 43,578.10 | 43,551.61 |
T(opt2) Greenhouse gas emissions from vehicle fleet (CO2-e(t) per 1,000 km)
| Apr 24 – Mar 25 | Apr 23 – Mar 24 | Apr 22 – Mar 23 | |
|---|---|---|---|
| CO2-e(t) per 1,000 km | 0.61 | 0.60 | 0.62 |
Total energy
E1 Total energy usage from fuels, including stationary fuels (F1) and transport fuels (T1) (MJ)
| Apr 24 – Mar 25 | Apr 23 – Mar 24 | Apr 22 – Mar 23 | |
|---|---|---|---|
| Total energy usage from stationary fuels (F1) (MJ) | 1,279,245.15 | 1,493,367.33 | 2,151,495.51 |
| Total energy usage from transport (T1) (MJ) | 370,674,749.20 | 375,172,272.10 | 384,343,471.40 |
| Total energy usage from fuels, including stationary fuels (F1) and transport fuels (T1) (MJ) | 371,953,994.35 | 376,665,639.43 | 386,494,966.91 |
E2 Total energy usage from electricity (MJ)
| Apr 24 – Mar 25 | Apr 23 – Mar 24 | Apr 22 – Mar 23 | |
|---|---|---|---|
| Total energy usage from electricity (MJ) | 28,891,285.39 | 28,625,723.94 | 30,453,184.21 |
E3 Total energy usage segmented by renewable and non-renewable sources (MJ)
| Apr 24 – Mar 25 | Apr 23 – Mar 24 | Apr 22 – Mar 23 | |
|---|---|---|---|
| Renewable | 28,891,283.73 | 28,625,725.82 | 24,350,365.32 |
| Non-renewable (E1 + E2 – E3 Renewable) | 371,953,996.01 | 376,663,017.45 | 392,597,785.79 |
E4 Units of Stationary Energy used normalised: (F1+E2)/normaliser
| Apr 24 – Mar 25 | Apr 23 – Mar 24 | Apr 22 – Mar 23 | |
|---|---|---|---|
| Energy per unit of Cases (MJ/Cases) | 34.86 | 34.77 | 39.64 |
| Energy per unit of floor space (MJ/m2) | 194.83 | 195.26 | 197.82 |
Sustainable buildings and infrastructure
| B1 Discuss how environmentally sustainable design (ESD) is incorporated into newly completed entity-owned buildings | A set of guidelines has been developed for the construction of ambulance branches, known as the Branch Design Guidelines. In 2021 sustainability options were identified and included as an addendum to the Branch Design Guidelines. There have been no changes to this process in 2023-24. |
| B2 Discuss how new entity leases meet the requirement to preference higher-rated office buildings and those with a Green Lease Schedule | Higher-rated sustainable office buildings are preferred for lease when the option is available. For example, when sustainability is considered alongside requirements such as location. |
| B3 NABERS Energy (National Australian Built Environment Rating system) ratings of newly completed/occupied Entity-owned office buildings and substantial tenancy fit-outs (itemised) | There were no newly completed/occupied entity-owned office buildings or substantial tenancy fir-outs. |
| B4 NABERS Energy – Environmental performance ratings (e.g. NABERS, Green Star, or ISCAIS rating scheme) of newly completed Entity-owned non-office building or infrastructure projects or upgrades with a value over $1 million | There were no newly complete entity-owned non-office building or infrastructure projects or upgrades with a value over $1 million. |
| B5 Rating scheme – Environmental performance ratings achieved for Entity-owned assets portfolio segmented by rating scheme and building, facility, or infrastructure type, where these ratings have been conducted | No environmental performance ratings were conducted. |
Water use
W1 Total units of metered water consumed by water source (kL)
| Apr 24 – Mar 25 | Apr 23 – Mar 24 | Apr 22 – Mar 23 | |
|---|---|---|---|
| Potable water (kL) | 34,319.14 | 32,218.23 | 31,956.74 |
| Total units of water consumed (kL) | 34,319.14 | 32,218.23 | 31,956.74 |
W2 Units of metered water consumed normalised by FTE, headcount, floor area, or other entity or sector specific quantity
| Apr 24 – Mar 25 | Apr 23 – Mar 24 | Apr 22 – Mar 23 | |
|---|---|---|---|
| Water per unit of Cases (kL/Cases) | 0.04 | 0.04 | 0.04 |
| Water per unit of floor space (kL/m2) | 0.22 | 0.21 | 0.19 |
Waste and recycling
WR1 Total units of waste disposed of by waste stream and disposal method (kg)
| Apr 24 – Mar 25 | Apr 23 – Mar 24 | Apr 22 – Mar 23 | |
|---|---|---|---|
| Landfill (total) | |||
| General waste – bins | 129,737.35 | 177,376.28 | 178,332.71 |
| General waste – skips | 50,756.74 | 111,645.48 | 95,062.84 |
| Offsite treatment | |||
| Clinical waste – incinerated | 1,684.90 | 1,580.08 | 4,154.76 |
| Clinical waste – treated | 53,166.49 | 103,212.71 | 149,373.23 |
| Recycling/recovery (disposal) | |||
| Batteries | 1,470.00 | 541.17 | 168.79 |
| Cardboard | 29,470.78 | 58,038.20 | 53,925.30 |
| Commingled | 34,490.66 | 261,067.95 | 231,263.23 |
| E-waste | 647.19 | 7,503.53 | 5,834.70 |
| Fluorescent tubes | 68.75 | 5.73 | |
| Grease traps | 47,864.00 | 4.15 | 9.67 |
| Organics (food) | 8,697.71 | 26,284.29 | – |
| Organics (garden) | – | 8,834.73 | 26,601.27 |
| Paper (confidential) | 5,354.21 | 12,663.83 | 16,914.22 |
| Paper (recycling) | – | 25,630.77 | 18,906.32 |
| Toner & print cartridges | – | 118.57 | 115.36 |
| Total units of waste disposed (kg) | 363,340.03 | 794,570.50 | 780,668.11 |
WR1 Total units of waste disposed of by waste stream and disposal method (%)
| Apr 24 – Mar 25 | Apr 23 – Mar 24 | Apr 22 – Mar 23 | |
|---|---|---|---|
| Landfill (total) | |||
| General waste | 49.68% | 36.37% | 35.02% |
| Offsite treatment | |||
| Clinical waste – incinerated | 0.46% | 0.20% | 0.53% |
| Clinical waste – treated | 14.63% | 12.99% | 19.13% |
| Recycling/recovery (disposal) | |||
| Batteries | 0.40% | 0.07% | 0.02% |
| Cardboard | 8.11% | 7.30% | 6.91% |
| Commingled | 9.49% | 32.86% | 29.62% |
| E-waste | 0.18% | 0.94% | 0.75% |
| Fluorescent tubes | – | 0.01% | 0.00% |
| Grease traps | 13.17% | 0.00% | 0.00% |
| Organics (food) | 2.39% | 3.31% | – |
| Organics (garden) | – | 1.11% | 3.41% |
| Paper (confidential) | 1.47% | 1.59% | 2.17% |
| Paper (recycling) | – | 3.23% | 2.42% |
| Toner & print cartridges | – | 0.01% | 0.01% |
WR2 Percentage of office sites covered by dedicated collection services for each waste stream
| Apr 24 – Mar 25 | Apr 23 – Mar 24 | Apr 22 – Mar 23 | |
|---|---|---|---|
| Printer cartridges | Not reported | ||
| Batteries | Not reported | ||
| E-waste | Not reported | ||
| Soft plastics | Not reported |
WR3 Total units of waste disposed normalised by FTE, headcount, floor area, or other entity or sector specific quantity, by disposal method
| Apr 24 – Mar 25 | Apr 23 – Mar 24 | Apr 22 – Mar 23 | |
|---|---|---|---|
| Total waste to landfill per Cases ((kg general waste)/Cases) | 0.21 | 0.33 | 0.33 |
| Total waste to offsite treatment per Cases ((kg offsite treatment)/Cases) | 0.06 | 0.12 | 0.19 |
| Total waste recycled and reused per Cases ((kg recycled and reused)/Cases) | 0.15 | 0.46 | 0.43 |
WR4 Recycling rate (%)
| Apr 24 – Mar 25 | Apr 23 – Mar 24 | Apr 22 – Mar 23 | |
|---|---|---|---|
| Weight of recyclable and organic materials (kg) | 127,994.55 | 400,755.94 | 353,744.57 |
| Weight of total waste (kg) | 363,340.03 | 794,570.50 | 780,668.11 |
| Recycling rate (%) | 35.23% | 50.44% | 45.31% |
WR5 Greenhouse gas emissions associated with waste disposal (CO2-e(t))
| Apr 24 – Mar 25 | Apr 23 – Mar 24 | Apr 22 – Mar 23 | |
|---|---|---|---|
| CO2-e(t) | 305.24 | 511.29 | 553.25 |
Greenhouse gas emissions
G1 Total Scope 1 (direct) greenhouse gas emissions (CO2-e(t))
| Apr 24 – Mar 25 | Apr 23 – Mar 24 | Apr 22 – Mar 23 | |
|---|---|---|---|
| Carbon Dioxide | 25,854.94 | 26,171.07 | 26,843.11 |
| Methane | 4.13 | 4.24 | 4.40 |
| Nitrous Oxide | 193.42 | 194.52 | 201.62 |
| Total | 26,052.48 | 26,369.82 | 27,049.13 |
| Scope 1 GHG emissions from stationary fuel (F2 Scope 1) (CO2-e(t)) | 67.46 | 78.90 | 113.65 |
| Scope 1 GHG emissions from vehicle fleet (T3 Scope 1) (CO2-e(t)) | 25,985.03 | 26,290.93 | 26,935.48 |
| Medical/Refrigerant gases | |||
| Methoxyflurane whistles | 17.21 | 13.14 | 14.68 |
| Total Scope 1 (direct) greenhouse gas emissions (CO2-e(t)) | 26,069.70 | 26,382.96 | 27,063.82 |
G2 Total Scope 2 (indirect electricity) greenhouse gas emissions (CO2-e(t))
| Apr 24 – Mar 25 | Apr 23 – Mar 24 | Apr 22 – Mar 23 | |
|---|---|---|---|
| Electricity | 5,019.74 | 5,015.16 | 5,642.17 |
| Electricity for Road Vehicles from Public or Private Chargers | 0.01 | ||
| Total Scope 2 (indirect electricity) greenhouse gas emissions (CO2-e(t)) | 5,019.74 | 5,015.17 | 5,642.17 |
G3 Total Scope 3 (other indirect) greenhouse gas emissions associated with commercial air travel and waste disposal (CO2-e(t))
| Apr 24 – Mar 25 | Apr 23 – Mar 24 | Apr 22 – Mar 23 | |
|---|---|---|---|
| Commercial air travel | 4.00 | 17.67 | 25.90 |
| Waste emissions (WR5) | 305.24 | 511.29 | 553.25 |
| Indirect emissions from Stationary Energy | 671.91 | 634.50 | 707.43 |
| Indirect emissions from Transport Energy | 15,251.55 | 667.95 | 753.93 |
| Paper emissions | 9.54 | 26.94 | 23.78 |
| Any other Scope 3 emissions | 56.47 | 54.10 | 55.49 |
| Total Scope 3 greenhouse gas emissions (CO2-e(t)) | 16,242.24 | 16,221.58 | 15,891.07 |
G(Opt) Net greenhouse gas emissions (CO2-e(t))
| Apr 24 – Mar 25 | Apr 23 – Mar 24 | Apr 22 – Mar 23 | |
|---|---|---|---|
| Gross greenhouse gas emissions (G1 + G2 + G3) (CO2-e(t)) | 47,330.96 | 47,565.62 | 48,607.82 |
| Electricity for Road Vehicles from Public or Private Chargers – Green Power Electricity | – | -0.02 | – |
| Green Power Electricity | -6,414.58 | -6,316.80 | -4,672.98 |
| Any Reduction Measures Offsets purchased (EL4-related) | -6,414.58 | -6,316.81 | -4,672.98 |
| Any Offsets purchased | -6,414.58 | -6,316.81 | -4,672.98 |
| Net greenhouse gas emissions (CO2-e(t)) | 40,916.37 | 41,248.81 | 43,934.84 |
Normalisation factors
| Apr 24 – Mar 25 | Apr 23 – Mar 24 | Apr 22 – Mar 23 | |
|---|---|---|---|
| 1000km (Corporate) | 9,288.36 | 9,430.88 | 9,400.55 |
| 1000km (Non-emergency) | 2,625.87 | 2,916.89 | 2,750.80 |
| 1000km (Road ambulance) | 31,008.71 | 31,230.33 | 31,400.26 |
| Aged Care OBD | – | – | – |
| Cases | 865,556.00 | 866,145.00 | 822,562.00 |
| Contractor | – | – | – |
| ED Departures | – | – | – |
| FTE | 6,195.77 | 6,167.00 | 6,270.00 |
| Flying hour (Fixed) | 5,373.46 | 5,790.69 | 5,684.32 |
| Flying hour (Rotary) | 3,323.02 | 3,602.07 | 3,668.75 |
| LOS | – | – | – |
| Non Departmental VPS Staff | – | – | – |
| OBD | – | – | – |
| PPT | – | – | – |
| Separations | – | – | – |
| TotalAreaM2 | 154,858.60 | 154,251.36 | 164,816.77 |
| Patient transport (ambulance road) | 736,094.00 | 717,883.00 | 689,360.00 |
| Patient transport (fixed air) | 4,813.00 | 2,817.00 | 5,467.00 |
| Patient transport (non-emergency road) | 120,339.00 | 143,510.00 | 125,313.00 |
| Patient transport (rotary air) | 4,310.00 | 1,935.00 | 2,422.00 |
Social procurement
Through our buying power, we generate social, economic and environmental outcomes that benefit the Victorian community and the environment. AV’s Social Procurement Framework provides the basis of our collaboration with our suppliers, to improve the social and environmental value of our purchasing decisions.
AV’s approach to social procurement is grounded by nine objectives, based on the Victorian Government’s Social Procurement Framework objectives.
These objectives are considered in purchasing decisions to deliver the social and environmental value we strive for, and include:
- Providing opportunities for Victorian Aboriginal people.
- Providing opportunities to Victorians with disability.
- Providing opportunities for disadvantaged Victorians.
- Engaging social enterprises, Australian disability enterprises and Aboriginal businesses where possible.
- Environmentally sustainable outputs through donations supporting a circular economy.
Key framework activity
AV’s social procurement activity resulted in engagements including uniforms, traffic management, employment services, facility services, IT equipment recycling, and catering services. These procurements also spanned the breadth of social procurement framework objectives.
Key framework achievements
AV’s Indigenous supplier spend with Supply Nation registered suppliers was $0.294 million and non-registered Indigenous supplier spend was $0.017 million. Our main Indigenous supplier provides AV uniforms to our paramedics and staff.
Another key outcome for AV is our partnership with Enable Social Enterprises. This partnership contributes significantly to the circular economy and environment while employing Victorians from areas experiencing high unemployment.
Table 1
| Aboriginal supplier spend by quarter (first and second tier) | 2025 FY Q1 | 2025 FY Q2 | 2025 FY Q3 | 2025 FY Q4 | Total |
|---|---|---|---|---|---|
| Aboriginal Supplier Spend | $113,964 | $90,888 | $66,903 | $22,326 | $294,081 |
Table 2
| Direct Social Procurement Spend (Direct) | Apr 24 – Mar 25 | Apr 23 – Mar 24 | Apr 22 – Mar 23 |
|---|---|---|---|
| Social procurement spend | $30.3m | $20.7m | $21.3m |
| Social procurement 'addressable spend' | $0.3m | $0.3m | $1.1m |
| Number of social suppliers* | 93 | 88 | 86 |
Enable Social Enterprises
Just over three years ago, we found that our storage areas for obsolete IT equipment were at capacity and additional space was needed for upcoming projects.
The AV Procurement, Sustainability and IT teams came together to investigate viable options to donate this surplus old equipment, allowing us to regain valuable storage space while acting in an environmentally sustainable way and supporting the community.
For the past three years, we have engaged Enable Social Enterprises (Enable) as our main source for the donation of obsolete equipment. Enable is a leading and award-winning not-for-profit social enterprise which tackles disadvantage and the digital divide by connecting community, environment and local economies.
The company employs young people with disabilities, people newly arrived to Australia, and people living in regions of high unemployment.
Enable facilitates the disassembly, sorting and dispatching of parts and commodities, as well as testing and refurbishment of computer equipment, and other services.
In 2024-25, we donated 4,685kg of goods to Enable, diverting it away from landfill and providing 173 hours of full award wage employment.
Emergency procurement
Nil to report.
Donations summary
General donations and bequests greater than or equal to $1,000
| Name of donor | Donation amount |
|---|---|
| Anonymous | $99,741.33 |
| Estate of Margaret Elaine Walker | $84,596.01 |
| Estate of Rachel Magda Hornung | $52,164.17 |
| Anonymous | $50,000.00 |
| Mr Christopher King | $40,000.00 |
| Anonymous | $20,000.00 |
| Copulos Foundation | $20,000.00 |
| Ritchies IGA | $16,386.48 |
| B.J. Davies OAM | $10,000.00 |
| Alma Sylvia & Carmen Figuerola Trust | $9,659.79 |
| Anonymous | $7,000.00 |
| Equity Trustees Charitable Foundation – The Dr David & Jennifer Komesaroff Trust | $6,666.00 |
| Eva May Foundation | $6,500.00 |
| Theo & Maureen Versteden | $5,000.00 |
| Anonymous | $4,999.11 |
| Anonymous | $4,719.21 |
| Anonymous | $3,700.00 |
| Anonymous | $3,600.00 |
| Craigieburn CERT | $3,186.94 |
| Freemasons Foundation Victoria | $3,142.00 |
| John Brian Little | $3,000.00 |
| Anonymous | $3,000.00 |
| Anonymous | $2,685.60 |
| Anonymous | $2,500.00 |
| OneTomorrow Charitable Fund | $2,376.00 |
| Anonymous | $2,350.00 |
| Lions Club of Yarrawonga | $2,000.00 |
| Anonymous | $2,000.00 |
| Daniela Frzovic (in honour of Radojka Frzovic) | $2,000.00 |
| Geraldine Jones (in Memory of Colin Jones) | $1,600.00 |
| Anonymous | $1,500.00 |
| Anonymous | $1,430.00 |
| Twice Blessed Op Shop Yarram | $1,300.00 |
| Anonymous | $1,200.00 |
| Anonymous | $1,011.50 |
| Community Bank Toora & Foster | $1,000.00 |
| CWA Benambra District | $1,000.00 |
| Anonymous | $1,000.00 |
| Lions Club of Nillumbik | $1,000.00 |
| Anonymous | $1,000.00 |
| M M Pettigrew | $1,000.00 |
| Anonymous | $1,000.00 |
| Anonymous | $1,000.00 |
| Anonymous | $1,000.00 |
| Anonymous | $1,000.00 |
| Anonymous | $1,000.00 |
| Anonymous | $1,000.00 |
| Anonymous | $1,000.00 |
| Joan Spiller | $1,000.00 |
| Sin Fong Chan | $1,000.00 |
| Angeline Chan | $1,000.00 |
| Total | $497,014.14 |
| General donations and bequests under $1,000 | $389,741.31 |
| Total general donations | $886,755.45 |
Auxiliary donations greater than or equal to $1,000
| Name | Auxiliary | Amount |
|---|---|---|
| Gippsland Wool Growers, Elders Rural | Helimed 1 | $10,652.28 |
| Paynesville Lions Club | Paynesville | $10,000.00 |
| Mallacoota Ambulance Auxiliary | Mallacoota | $5,000.00 |
| Ritchies | Paynesville | $3,673.09 |
| Stratford Lions Club | Helimed 1 | $3,500.00 |
| Raymond Island Tai Chi Group | Paynesville | $3,000.00 |
| Nicholas Johns Op Shop | Lakes Entrance | $2,500.00 |
| R C Wheeler | Maffra | $2,500.00 |
| Parkridge Social Club | Paynesville | $2,500.00 |
| Cheque Deposit | Beaufort | $2,000.00 |
| Barb Merlihan | Loch Sport | $1,341.00 |
| Fitz Cheque | Beaufort | $1,000.00 |
| St J's Opp Shop | Maffra | $1,000.00 |
| Paynesville Uniting Church Op Shop | Paynesville | $1,000.00 |
| Total | $ 49,666.37 | |
| Auxiliary donations and bequests under $1,000 | $119,534.51 | |
| Total auxiliary donations | $169,200.88 |
Governance
AV Charter
AV aims to improve the health of the community by providing high quality pre-hospital emergency care and medical transport. We service a population of over six million people annually.
AV is a statutory authority required by the Ambulance Services Act 1986 to provide state-wide emergency pre-hospital ambulance services to all Victorians. This includes to:
- Respond rapidly to requests for help in a medical emergency.
- Provide specialised medical skills to maintain life and to reduce injuries in emergency situations and while transporting patients.
- Provide safe, patient-centred and appropriate services.
- Provide specialised transport facilities to move people requiring emergency medical treatment.
- Provide services for which specialised medical, or transport skills are necessary.
- Foster continuous improvement in the quality and safety of the care and services it provides.
- Foster public education in first aid.
AV was established on 1 July 2008 following the merger of the Metropolitan Ambulance Service, Rural Ambulance Victoria and the Alexandra and District Ambulance Service.
AV reports to the Hon. Mary-Anne Thomas MP, Minister for Ambulance Services.
Appointed by the Governor in Council on the recommendation of the Minister, the Board of Directors (the Board) is responsible for the provision of comprehensive, safe and efficient ambulance services to the people of Victoria.
While organisational operations and management is vested in the Chief Executive Officer and the Executive team, the Board is accountable to the Victorian Government and Minister for the overall and ongoing performance of AV.
The Board operates in accordance with the AV By-Laws (approved by the Department of Health Secretary), as well as other Board and government policies and frameworks. These support AV to meet its statutory obligations and, in doing so, comply with appropriate standards of governance, transparency, accountability and propriety. All Board and committee members are independent, non-executive Directors.
The Board’s qualifications, skills and experience are diverse and extensive, with expertise across government, technology and transformation, finance, accounting, law, commerce, diversity, leadership, governance, not-for-profit settings, community engagement, and culture.
The Board also ensures it maintains regular engagement with representatives of other health services, government department officers, external specialists and other Board Chairs to ensure it remains connected to contemporary practices and initiatives in health, risk and governance.
The Board Chair works with DH and the Minister to ensure the Board has the requisite skills, competency and diversity mix to provide strong and insightful stewardship of the organisation.
This includes ensuring the Board has the attributes required not only for today’s needs, but also for future years where the Board will need to respond to a more technologically, financially and socially complex environment and ensuring that AV is safe, fair and inclusive.
Board Committees
The Board maintains three statutory committees, two advisory committees, and a Remuneration and Nominations Committee to support its functions.
All committees are governed by Board-approved Terms of References, which set out each committee’s role, responsibilities, membership, quorum and voting structures. The Board appoints all committee members (reviewed annually) and ensures annual performance and effectiveness reviews are conducted and reported.
Committee activities continue to be periodically reviewed, to ensure they remain fit-for-purpose, aligned to legislation and government frameworks and best practice governance, and advance the Board’s role and responsibilities under the Ambulance Services Act 1986.
The Board’s qualifications, skills and experience are diverse and extensive, with expertise across government, technology and transformation, finance, accounting, law, commerce, diversity, leadership, governance, not-for-profit settings, community engagement, and culture.
Finance Committee (section 18 requirement)
The Finance Committee advises the Board on AV’s financial and business plans, strategies and budgets to ensure the long-term financial viability of the organisation. The committee assists the Board in monitoring strategies that seek to maximise revenue, and the effective and efficient use of AV financial resources and assets. Specific responsibilities include:
- Financial strategy.
- Financial reporting.
- Business and financial planning and performance.
The committee is assisted in its work by the extensive commercial, finance and accounting experience of its members, including an independent member. The committee continuously improves its insights into AV through regular presentations on key areas of the business which present both financial opportunity and challenge for the organisation.
Audit and Risk Committee (section 18 requirement)
The Audit and Risk Committee assists the AV Board in fulfilling its responsibilities in the areas of compliance, internal control, financial reporting, assurance activities and contemporary risk management.
Specific responsibilities include:
- Financial risk and internal controls.
- Financial reporting and management.
- Internal and external audit.
- AV’s compliance with laws, regulations, internal policies and industry standards.
- Enterprise risk management (sharing responsibility with the Quality and Safety Committee in overseeing clinical risks).
Throughout the year, the committee regularly engaged with AV’s internal auditors (Ernst & Young) and external auditors (Victorian Auditor General’s Office). This ensured the committee provided the Board and AV with robust and informed oversight of matters mandated by its Terms of Reference, the Department of Health, and the Department of Treasury and Finance.
The committee’s work is supported by a strong cross-section of skills and experience.
The committee continues to update and refine AV’s risk and risk appetite framework, as well as staying connected to internal and external emerging risks. In 2024-25, the committee continued its oversight of material risks including, but not limited to, the ICT, security, patient safety, privacy and organisational culture.
Quality and Safety Committee (section 18 requirement)
The Quality and Safety Committee is responsible to the Board for monitoring the performance of AV with regard to whether:
- Effective and accountable systems are in place to monitor and improve the quality, safety and effectiveness of services provided by AV.
- Any systemic problems identified with the quality, safety and effectiveness of ambulance services are addressed and the results reported in a timely manner.
- AV continuously strives to improve the quality of the services it provides and to foster innovation.
The committee actively monitors the performance of quality care and service provision against the five domains of the Safer Care Victoria Clinical Governance Framework and AV’s own Best Care Framework.
Membership includes AV Directors (each with clinical governance, health service and legal and experience), paramedic observers and Community Advisory Committee members.
The committee maintains an ongoing commitment to evolving its knowledge and consideration of new clinical governance practices and frameworks, comprehensive quality and safety reporting, and ways to effectively monitor and measure patient care, safety and experience.
This is supported by the connection of its directors to emerging best practices across public health generally, as well as the advancements in data and clinical practices delivered by management.
Patient case examples remain a consistent part of this committee’s work plan, to provide members with a direct connection to patient experiences, AV clinical practices and clinical governance performance.
People and Culture Committee
The People and Culture Committee advises the Board on material policies and strategies to improve the health, safety, wellbeing, development and performance of AV employees. The committee monitors the development and implementation of strategies to ensure the organisation fosters and promotes a positive culture that enables delivery of high-quality patient care, and a safe and supportive environment for all employees.
The committee’s focus remains workforce health, safety, workplace cultural programs, employee engagement, emerging technology practices relevant to manual handling, strategic workforce planning, and other initiatives that drive a safer, fairer, more inclusive work environment for our people.
Prior to the closure of the YourAV program, the committee supported the implementation and embedding of the recommendations made by the Victorian Equal Opportunity and Human Rights Commission in its independent review. In 2025, the committee continues its focus on building a respectful and safe workplace by overseeing the roll-out of the AV People Plan.
In 2024-25, the committee further enhanced their skills and expertise with the inclusion of a new independent committee member.
Community Advisory Committee
The Community Advisory Committee (CAC) informs and guides the Board and Executive on key issues associated with AV’s work with the community.
Independent community members come from a diverse range of backgrounds, experience and education sets and have been an important part of the CAC’s successful contribution to service design planning and AV’s patient care commitments.
In 2024-25 we recruited new members to the Committee who are providing us with invaluable contributions that strengthen voice of the community in our service design processes and decision making.
Led by an Independent member Chair in 2024-25, the CAC has become a valued source of patient, consumer, and community insights as to how we can better deliver our services.
Through engagement with our CAC, we have developed the Community and Consumer Engagement Plan which they continue to monitor. Throughout 2024-25, the CAC also participated in various service design workshops and provided advice on:
- Open Disclosure and Statutory Duty of Candour Procedure
- Patient Experience Insight Enhancements
- National Safety and Quality Health Service Standards
- Social Procurement
- Community Fundraising
- Timely Emergency Care 2 (TEC2) Improvement Program
- Community Forums, and
- AV’s Disability Inclusion Program.
Board Director profiles
Board Chair
Shelly Park
Appointed 26 August 2022
Ms. Park has more than 25 years in CEO and senior executive roles and in governing complex organisations.
She has extensive experience and knowledge of high-performing Boards and brings a broad strategic focus to her role as a non-executive director, ensuring organisations deliver commercial outcomes and perform to ethical standards.
Ms. Park brings strengths in financial stewardship, is an experienced crisis leader and demonstrates passion for quality, leadership, safety and risk governance. Her work is informed by deep experience in leading turnaround strategies and transformations in large and complex health/life science related organisations (including business processes, automation, technology, digital and ICT security).
She also has a strong passion for leadership, strong stakeholder engagement (including Government and regulatory bodies) and has achieved strategic outcomes in highly complex and regulated environments. Ms. Park has a strong track record of delivering strategic goals by applying her understanding of the voice of the patient, clinical and professional leadership, people leadership, and embedding governance frameworks.
Board Members
Andrew Crisp AM APM
Board Member (July 2024 – August 2024)
Andrew served a distinguished 40-year career with Victoria Police where he held a number of senior executive positions, finishing in the role of Deputy Commissioner Regional Operations. In 2018, Andrew was appointed as Victoria’s Emergency Management Commissioner, a position he held for five years.
In these roles Andrew provided strong leadership and was a calm, familiar face for Victorians during some of the most significant emergencies the state has faced including the 2019-20 bushfires and the COVID-19 pandemic response.
In both his police and emergency services roles, Andrew is regarded as someone with sound judgement who builds effective teams that deliver positive outcomes for the Victorian community. It is important to Andrew that all voices are listened to, and that inclusion and diversity are front of mind when it comes to organisational culture and service delivery.
Andrew is well known as a champion for multicultural and faith communities and firmly believes he is a better person and leader through those relationships. Andrew joined the Board of AV in July 2024, then took a leave of absence from his role as a director to undertake the role of Interim CEO at AV from the 21 August, 2024 to 30 June 2025.
Andrew will return as Chair of the AV Board from 1 July 2025.
Dr Fergus Kerr
MBBS, FACEM, MPH, FRACMA, GAICD
Appointed July 2024
Fergus Kerr joined the Royal Melbourne Hospital as Chief Medical Officer in 2022, having been Group Director of Medical Services and Clinical Governance at Cabrini Health in Melbourne. Fergus was appointed as an Emergency Physician and Toxicologist at Austin Health in 1997.
10 years later, in September 2007, he undertook a new challenge as Director of Emergency Medicine, and in 2011 he extended his leadership roles by taking up the Medical Directorship of the Medical and Emergency Clinical Services Unit.
More recently, in a desire to develop his leadership capacity formally, Fergus completed his Fellowship with the Royal Australasian College for Medical Administrators following which he took up the role as the Executive Director of Medical Services at Peninsula Health.
In 2016 Fergus returned to Austin Health in an Executive position as the Chief Medical Officer. He has a strong interest in Toxicology, spending two years undertaking specialist training at the University of Pittsburgh and was pivotal in establishing the Victorian Poisons Information Centre at Austin Health. He has previously been an examiner with the Australasian College for Emergency Medicine and, up until January 2018, continued to practice clinically.
Wenda Donaldson
Appointed July 2020
Wenda is a public sector and not-for-profit senior executive, combining her non-Executive Board career with her role as Chief Operating Officer at Key Assets Australia, a national children’s and family services agency.
Wenda has held executive roles with Uniting Vic.Tas, Australian Red Cross, Australian Department of Education and the Australian Sports Commission.
Wenda has proven expertise in advocacy for policy reform and investment to enhance outcomes for those experiencing vulnerability or disadvantages. She has also been involved in the establishment of inter-governmental and multi sector partnership agreements to deliver on major public policy reforms.
Denise Heinjus OAM
Appointed July 2023
Denise is an experienced leader in driving positive cultural and clinical change for the mutual benefit of an organisation, its people, and the community.
Denise was Executive Director of Nursing at the Royal Melbourne Hospital (RMH) for 16 years prior to her retirement in 2022. Preceding her appointment at RMH, she held similar roles as Executive Director of Nursing and Midwifery at Monash Health, Illawarra Area Health Service and Northern Sydney Central Coast. Her roles have included managing nursing services, workforce and education, residential aged care, allied health services, Aboriginal health and emergency management.
Denise is passionate about shaping ‘just’ workplace cultures, in which an organisation’s people thrive as individuals and team members. Throughout her career, she has worked closely with employees and volunteers to create strategies, procedures and resources to minimise harm from occupational violence and sexual harassment.
Allison Smith
B.Acc, GAICD, CA (Australia and Scotland)
Appointed July 2024
With extensive experience in multiple industries, Allison is recognised as a leader in a number of disciplines, but specifically financial analysis and reporting. She has held senior finance, retail, merchandise, marketing, supply chain and IT roles in some of Australia’s most influential organisations.
Allison has a passion for innovation and cultural enhancement in the public health and emergency services sectors.
She is also a Board Member of the Victorian Institute of Forensic Mental Health where she chairs the Finance and Capital Works Committee. She was previously the Deputy Chair of Peninsula Health where she was also Chair of the Finance, Resource and Capital works Committee and a member of the Audit and Risk Committee, People & Culture Committee and the Remuneration & Nominations Committee.
She is a member of the Australia & New Zealand Institute of Chartered Accountants and a Graduate of the Australian Institute of Company Directors.
Allison has previously been an independent member of the AV Board’s Audit and Risk Committee.
Vijaya Vaidyanath
Appointed July 2022
Vijaya Vaidyanath is the former CEO of Homes Melbourne – a special entity of City of Melbourne. Prior to this role, Vijaya was the CEO of City of Yarra in Melbourne from July 2012 – January 2022. Vijaya spent over a decade as CEO at Waitakere City Council and as the CEO of Rodney District Council in New Zealand. She is a Board Member at Procurement Australia, Parks Victoria, AV and Vision Super, and former Board member of Zoos Victoria.
Vijaya’s exemplary qualifications include a Senior Executive Fellow of the John F Kennedy School of Government, Harvard University, MBA from JMKatz Graduate School of Business in Pittsburgh USA, Master of Arts (Economics) and a Bachelor of Arts (Economics) from the University of Bangalore.
Vijaya draws inspiration from a variety of global thought and academic leaders as well as from her overseas mentors who have shaped her world view and led to her interest in social justice and values-based leadership. She has been a leader from the very early stages of her career in sectors such as commercial and central banking, international finance, and local government in both New Zealand and Australia.
Vijaya is renowned for her innovation, integrity, inspiring leadership style and a unique ability to deliver results. She instils a strong sense of pride and passion in her staff who deliver exemplary outcomes for our communities. Her strong belief in building coalitions and harnessing community capacity has been her work philosophy.
Dipak Sanghvi
Appointed July 2022
Mr. Dipak Sanghvi is a pharmacist and pharmacy owner in Victoria and is currently Board Chair of Musculoskeletal Australia and Monash Health.
His previous positions include President of the Pharmacy Guild Victoria Branch 2006-2011, Board Chair of Gold Cross Products and Services Pty Ltd, Board Chair of Return of Unwanted Medicines, Board member of Guild Insurance and Superannuation and Meridian Lawyers, as well as several other board positions both in the community and the pharmaceutical industry.
Amanda Watt
BCom LLB (Hons) LLM GAICD MAPP
Appointed July 2022
Amanda has extensive expertise in employment, industrial, and equal opportunity law.
During Amanda’s 30-year plus experience advising the public and private sectors across many industries, including health and education, she has worked with clients on embedding strategic and sustainable workplace solutions. She has a comprehensive understanding of risk management, employee relations and culture.
Amanda also has a deep appreciation of the human, societal and economic impact of systemic sexual harassment and discrimination in our workplaces.
She was a contributor to the Champions of Change Coalition’s report: Disrupting the System – preventing and responding to sexual harassment in the workplace and has supported the work of the Respect@Work Council on its best practice guidance for confidentiality agreements.
Amanda has been independently recognised by Best Lawyers in the areas of Employee Benefits, Labour and Employment, Government, and Education, and as a leading individual in Employment Law by the Legal 500 Asia Pacific.
Amanda Chairs the Audit and Risk Committee and is a member of the People and Culture Committee.
Board diversity
| No | Yes | |
|---|---|---|
| Aboriginal and Torres Strait Islander | 100% | 0% |
| No | Yes | |
|---|---|---|
| Cultural and linguistically diverse background | 62.5% (5) | 37.5% (3) |
| No | Yes | |
|---|---|---|
| Identify as a person with a disability | 89.8% (8) | 11.11% (1) |
| Man | Woman | |
|---|---|---|
| Gender | 33.33% (3) | 66.67% (6) |
| 45-54 | 55-64 | 65+ | |
|---|---|---|---|
| Age | 11.11% (1) | 33.33% (3) | 55.56% (5) |
| Metro | |
|---|---|
| Principal place of residence | 100% |
Board meetings
| Board | Finance Committee | Audit & Risk Committee | Quality & Safety Committee | People & Culture Committee | Community Advisory Committee | Rem & Nom Committee | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Chair | S. Park | A. Smith | D. Sanghvi & A. Watt | Dr F. Kerr | W. Donaldson | C. Furlanetto OAM | S. Park | |||||||
| Board of Directors | H | A | H | A | H | A | H | A | H | A | H | A | H | A |
| S. Park (AV Chair) | 15 | 15 | Ex Officio | 5 | Ex Officio | 2 | Ex Officio | 2 | Ex Officio | 2 | Ex Officio | 2 | 4 | 4 |
| W. Donaldson | 15 | 15 | 4 | 4 | 5 | 5 | ||||||||
| D. Heinjus OAM | 15 | 13 | 5 | 5 | 5 | 5 | ||||||||
| F. Kerr | 15 | 15 | 9 | 9 | 5 | 5 | ||||||||
| D. Sangvhi | 15 | 12 | 2 | 2 | 5 | 2 | 3 | 3 | 4 | 4 | ||||
| A. Smith | 15 | 13 | 9 | 9 | 4 | 3 | 5 | 4 | ||||||
| V. Vaidyanath | 15 | 15 | 9 | 8 | 4 | 3 | 4 | 4 | ||||||
| A. Watt | 15 | 14 | 3 | 3 | 1 | 1 | ||||||||
| A. Crisp | 5 | 5 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 |
| Rod Maule (People and Culture Committee Independent Member) | 5 | 5 | 1 | 1 | ||||||||||
| Kathryn Brown (Finance Independent Member) | 9 | 7 | ||||||||||||
| D. Cudini# | 1 | 1 | ||||||||||||
| T. Rodda# | 1 | 1 | ||||||||||||
| C. Furlanetto OM | 4 | 3 | ||||||||||||
| Kane Treloar^ | 5 | 3 | 4 | 4 | ||||||||||
| Cara Hudson^ | 4 | 4 | ||||||||||||
| Mumtaz Aktar^ | 4 | 2 | ||||||||||||
| Laura Collister ^ | 4 | 4 | ||||||||||||
| R. Coverdale^^ | 4 | 4 | ||||||||||||
| Baruch Goberman^ | 4 | 3 | ||||||||||||
| Pauline Rogers ^ | 4 | 4 | ||||||||||||
Notes
H = Meetings eligible to attend (excludes those held by circular resolution) vs A = meetings attended
* Includes one (1) joint meeting.
** Includes two (2) joint meetings.
^ Community members of the Community Advisory Committee.
^^ R Coverdale & K Treloar are also voting members of Quality & Safety Committee.
# Paramedic representative (no voting rights).
Executive group
Chief Executive Officer
Jordan Emery Appointed 30 June 2025
Andrew Crisp Interim 21 August 2024 – 29 June 2025
Jane Miller until 20 August 2024
With the following acting arrangements during periods of leave:
Danielle North Acting 9 September 2024 – 29 September 2024
Anthony Carlyon Acting 30 April 2025 – 09 June 2025 Acting 30 September 2024 – 24 October 2024 Acting 29 August 2024 – 08 September 2024
Responsible to the Board of Directors for the overall management and performance of AV.
Chief Information Officer
Gavin Gusling As at 30 June 2025
Responsible for digital strategy, digital and technology innovation, cyber security, organisational wide data and reporting and insights.
Development of systems architecture, major system changes or introduction / integration of new systems, master data management and data governance.
Also responsible for data sharing agreements, ongoing maintenance of applications and infrastructure and hardware, including real-time support for IT end-users consistent with our service level objectives.
The Business Technology and Programs Division is also responsible for organisational Change management and all enterprise-wide program and project delivery.
Executive Director Enterprise Services
Jesse Maddison Acting April to June 2025
Jodie Gilbert Acting March to April 2025
Travis Heeney January to March 2025
Garry Button Until January 2025
Responsible for providing capabilities across the organisation to both corporate and operational departments.
Enterprise Services supports AV’s accountability to the Victorian Government, and is responsible for providing financial, procurement and legal advice, managing corporate and operational risk, strategic planning, the AV Membership Subscription Scheme and equipping operational staff to best service the community
Executive Director People and Culture
Jesse Maddison Appointed October 2024
Heather Miller Acting May 2025 – June 2025
Samira Richards Until September 2024
Responsible for providing leadership and direction for the organisation’s workforce strategy, organisational capability, wellbeing and safety and employee experience programs.
This includes leading the implementation of the organisation’s inaugural People Plan, focused on improvements in areas of diversity and inclusion, health and safety, wellbeing and support services, leadership and human resources and payroll systems.
Executive Director Quality and Clinical Innovation
Dr Tegwyn McManamny Appointed January 2025 Acting October 2024 – January 2025
Katherine Peck Acting July 2024 – October 2024
Responsible for providing leadership and direction for clinical governance, patient safety and quality systems, and support a culture of continuous improvement in the delivery of patient centred care to ensure AV delivers Best Care every time.
Executive Director Regional Operations
Danielle North As at 30 June 2025
Narelle Capp Acting 29 August – 29 September 2024
As the core operational division, Regional Operations is responsible for delivering quality, patient-focused emergency medical response and pre-hospital care to Victorians and cross border communities.
This is achieved through a variety of career, volunteer and co-responder service delivery models and a dedicated workforce of approximately 4,000 operational staff made up of Mobile Intensive Care (MICA) paramedics, Advanced Life Support (ALS) paramedics, Ambulance Community Officers (ACO), and Community Emergency Response Teams (CERT) supported by Remote Area Nurse and Firefighter co-responders across the state.
Executive Director Strategy and Engagement
Alison Errey As at 30 June 2025
Responsible for leadership of strategic internal and external communication; engaging with our people, partners, community and stakeholders in AV’s contemporary role in Victoria’s public health system.
Executive Director Specialist Operations and Coordination
Anthony Carlyon As at 30 June 2025
Andrew Keenan Acting 28 June 2025 – current Acting 1 May 2025 – 9 June 2025
Michael Georgiou Acting 29 August 2024 – 1 December 2024
The Specialist Operations and Coordination (SOC) division facilitates patient access by coordinating ambulance resourcing and providing support to our operational workforce on day to day operations.
This includes emergency and non-emergency ambulance response and facilitating access to alternate care pathways following secondary triage assessment.
SOC provides direct specialist care, and clinical advice to the Victorian community and health services through retrieval, aeromedical and stroke specialist services.
Chief Medical Officer
Dr David Anderson As at 30 June 2025
Dr Francesca Tullio Acting 26 July 2024 – 27 January 2025
Responsible for providing clinical leadership and specialist medical advice to the organisation. Oversees the development, implementation and evaluation of up-to-date evidence based clinical practices.
Contributes to the teaching of paramedics, provides both on scene and remote clinical support and advice to paramedics and responds to incidents as required, including selected complex patients and major incidents.
Statement of Priorities
AV’s Statement of Priorities is the key service delivery and accountability agreement between AV and the Victorian Government. This agreement facilitates delivery of, or progress towards, the government’s commitments for the financial year.
DH System Priority 1: Excellence in clinical governance
We aim for the best patient experience and care outcomes by assuring safe practice, leadership of safety, an engaged and capable workforce, and continuing to improve and innovate care.
Goals
- Continue to improve patient health outcomes and experiences by delivering timely, high-quality care and connecting patients to alternative services where safe and appropriate.
- Continue to learn, innovate and implement initiatives that improve the delivery of services and support better health outcomes for Victorians.
AV Deliverables
1
Engage with frontline staff to design, test and scale improvements that respond to the drivers of performance and support access to timely emergency care.
Associated Strategic Plan outcome
2.1 All patients receive best care, improved health outcomes and experience
Associated AV Annual Plan Initiative
Timely Emergency Care Program (TEC2)
AV Achievements
AV is continuing to engage with frontline staff as part of the Timely Emergency Care Program (TEC2), which is designed to empower those closest to our patients to lead improvements in care and performance in the areas of Daily Operating System, Transfer, Clearing, and Safe in Place. In 2024-25, 17 TEC 2 Plan-Do-Study-Act cycles were completed with strong attendance by operational staff at the TEC capability sessions.
2
AV will continue implementation of the Cardiac Arrest Improvement Strategy to drive improvements in patient care and survival rates over the next five years including:
- providing enhanced feedback to paramedics
- embedding opportunities for greater infield care, and
- better monitoring of patient outcomes and performance.
Associated Strategic Plan outcome
2.3 Our clinical response model and provision of care is constantly evolving and sets best practice standards
AV Achievements
In 2024-25 AV has released the Out-of-Hospital Cardiac Arrest Regional Report. The report provides clinical leaders across AV the opportunity to benchmark 40 resuscitation metrics and outcomes across regions, and to drill down to team-level outliers in performance that may help focus areas for debriefing and review.
AV has also launched a new campaign ‘Are you Resus Ready’ across Victoria to enhance paramedic preparedness to resuscitation cases.
3
AV will work with health service partners to implement strategies to improve access to timely pre-hospital care and system-wide patient flow.
This will include progressively increasing the use of alternative service pathways by promoting the use of the Victorian Virtual Emergency Department (VVED) and understanding and addressing barriers for using these services, and by using education and guidance to reduce conveyance rates to hospital.
Associated Strategic Plan outcome
2.1 All patients receive best care, improved health outcomes and experience
AV Achievements
AV has implemented strategies to promote use of VVED and other alternate services providers, including a streamlined and improved VVED referrals registration form, targeted education in Residential Aged Care Facilities to address concerns and barriers to its use, and uplift of pathways for vulnerable patient populations, including the introduction of Elder Rights Australia pathway.
AV is also continuing to promote referral pathways on the AV website as well as promotion and education of VVED by our in-field teams.
4
AV will continue to implement Best Care clinical governance framework which encompasses all elements of clinical/patient service delivery including alternative service pathways, ensuring that the patient climate supports safe, person-centred care and a quality patient experience.
Associated Strategic Plan outcome
2.1 All patients receive best care, improved health outcomes and experience
AV Achievements
In 2024-25 AV launched the Best Care, Everywhere Framework and is continuing to implement actions to ensure appropriate, person-centred, quality care is provided to our patients. This includes:
- developing and progressing a Clinical Quality Improvement Plan
- creation of a centralised clinical risk register and clinical quality improvement register
- progressed development of Best Care Performance Framework to enable outcome reporting of our Best Care Success Measures
- developed collaborative regional improvement register
- developed and distributed the Paramedic Exposure Analysis tool to provide an intuitive, rapid, and reproducible method for analysing paramedics' exposure to critical cases to inform improvement opportunities.
DH System Priority 2: Operate within Budget
Ensure equitable and transparent use of available resources to achieve optimum outcomes.
Goals
- Develop and implement an approach to deliver an end of financial year balanced operating result in partnership with the department with a goal to manage cost growth effectively to ensure the efficient operation of the health service
- Implement reforms that support financial sustainability.
AV Deliverables
1
AV will improve operational efficiency, capability in financial planning and analyses and the annual budgeting and forecasting processes. In 2024-25 this will focus on continuation of a financial budgeting and forecasting tool, and associated processes by March 2025, to support development of the 2025-26 budget.
Associated Strategic Plan outcome
3.1 Our organisation is efficient enabling us to deliver more impact to our community
Associated AV Annual Plan Initiative
Financial Sustainability Plan
AV Achievements
AV has developed financial planning and analysis improvements, and monthly forecasting in accordance with DH reporting requirements, with efficiencies expected to support future budget processes.
AV has been working with experts in health services finances to assist with our future financial sustainability including developing financial improvement plans.
2
AV will also:
- implement strategies to control costs, such as negotiating favourable contracts with suppliers, optimising workforce utilisation, and managing healthcare technologies and equipment effectively
- utilise data analytics and performance metrics to identify areas of inefficiency and waste, and make evidence-based decisions to improve financial sustainability and operational performance
- develop robust financial forecasting models to project future revenue and expenditure, identify financial risks, and implement risk mitigation strategies to ensure long-term sustainability
- explore opportunities to diversify revenue streams through partnerships, grants, research funding, and other innovative financing models to reduce dependence on government funding.
Associated Strategic Plan outcome
3.1 Our organisation is efficient enabling us to deliver more impact to our communit
Associated AV Annual Plan Initiative
Financial Sustainability Plan
AV Achievements
AV has negotiated favourable contractual terms with a large information technology supplier to deliver considerable cost savings. Fleet management initiatives undertaken in FY25 are also expected to deliver significant capital savings from FY26 onwards.
Research and investigation into the use of medical supplies has resulted in significant efficiencies, waste reduction, and savings The use of ambulance services to deliver non-clinically necessary services has also been analysed resulting in significant efficiencies and savings.
Forecasting models were used to identify significant financial risks associated with the impacts of the Protected Industrial Action on AV’s revenue. Strategies to minimise this risk included the establishment of data sharing agreements with over 20 major health services across Victoria.
The growth of AV’s microdonations through AV’s membership portal continues to deliver additional revenue for AV.
DH System Priority 3: Improving equitable access to healthcare and wellbeing
Ensure that Aboriginal people have access to a health, wellbeing and care system that is holistic, culturally safe, accessible, and empowering.
Ensure that communities in rural and regional areas can have equitable health outcomes irrespective of locality.
Goals
- Continue to strengthen AV’s commitment to ensure Aboriginal communities have access to culturally safe and sensitive services
- Strengthen cultural safety in the delivery of services
- Expand the delivery of high-quality cultural safety training for all staff to align with the Aboriginal and Torres Strait Islander cultural safety framework
- Improve access to services for rural and regional people, including through community based and virtual care, and
- Work with other system partners to optimise availability of ambulances and paramedic skills in rural and regional locations.
AV Deliverables
1
Progress implementation of AV’s ‘Reflect’ Reconciliation Action Plan (RAP) in accordance with agreed timeframes outlined in the Plan.
This Plan will help to strengthen relationships with Aboriginal and Torres Strait Islander stakeholders and improve cultural safety for the workforce and patients. In 2024-25, this will include:
- uplifting the capability of staff to support cultural safety of patients by implementing mandatory cultural safety training and assessment for all staff
- building knowledge and tools to support a more inclusive workplace, and
- supporting reconciliation events that demonstrate organisational solidarity with Aboriginal and Torres Strait Islander peoples and communities.
Associated Strategic Plan outcome
4.3: Our communities are resilient and informed
Associated AV Annual Plan Initiative
Reconciliation Action Plan
AV Achievements
AV has completed implementation of our ‘Reflect’ RAP and has developed our ‘Innovate’ RAP which will commence implemented in 2025-26.
Patient identity fields in VACIS relating to Aboriginal and Torres Strait Islander status are in the process of being made mandatory. Asking every patient if they identify as Aboriginal and/or Torres Strait Islander helps to create safer, more affirming experiences for Aboriginal and Torres Strait Islander peoples and link people in with the right care. Mandating this field in VACIS will also improve the quality of our data, helping us understand the needs of the people we care for.
Cultural recognition training is available to all staff. This training module incorporates strategies for working with Aboriginal and Torres Strait Islanders (both as co-workers and/or patients).
Aboriginal and Torres Strait Islander reference material is available to all staff.
AV proudly attends key Aboriginal events such as NAIDOC Week and National Reconciliation Week.
2
AV will continue to expand the use of the VVED and increase state-wide utilisation. This will include:
- promoting utilisation of VVED through AV’s Secondary Triage Service and via in-field referral from paramedics and other responders for all suitable patients; and
- ensuring continuous improvement of processes and systems associated with the safe use of virtual care, including providing staff and consumers with appropriate support and communications.
Associated Strategic Plan outcome
2.1 All patients receive best care, improved health outcomes and experience
AV Achievements
For non-life-threatening conditions, AV encourages the community, secondary triage practitioners and paramedics in-field to utilise the VVED. VVED has continued to be promoted via the AV public facing website with targeted in-field education of Residential Aged Care Facilities.
In 2024-25, the Secondary Triage team expanded use of Video Assisted Triage. This service enables expert nurses and paramedics to better assess patients and connect them with the most appropriate care. This is an Australasian first, and ensures ambulances are available for the most critically ill patients. Being able to both see and hear the patient has been a significant innovation for the AV triage services team and is resulting in increased utilisation of alternate service providers, including VVED.
3
Support the development and delivery of Paramedic Practitioners in rural and regional Victoria, in line with the government’s election commitment.
Associated Strategic Plan outcome
2.2 Remote and marginalised cohorts have better access to healthcare and improved health outcomes
Associated AV Annual Plan Initiative
Paramedic Practitioner
AV Achievements
AV is continuing to support establishment of the new Paramedic Practitioner role within rural Victoria by December 2026.
AV is working closely with the Department of Health, Safer Care Victoria and Monash University and other key stakeholders to help design this innovative role, agreeing the service delivery model and drafting the scope of practice.
The first cohort of students who commenced the Paramedic Practitioner course in 2024 are now undertaking their second year of the three-year degree which includes clinical placements. In February 2025, the second cohort of 26 students commenced their studies, expanding the number of overall practitioners available to step into advanced practitioner roles.
4
AV will work with the Country Fire Authority (CFA) to continue to implement the Fire Medical Response (FMR) program. The program is being developed to align with the Emergency Medical Response program and aims to utilise Country Fire Authority (CFA) people to provide rapid responses and specific treatment to targeted medical emergencies including Priority Zero responses.
Associated Strategic Plan outcome
2.2 Remote and marginalised cohorts have better access to healthcare and improved health outcomes
AV Achievements
AV is continuing to work with CFA to implement the FMR program, which was developed to align with AV’s commitment to improve out of hospital cardiac arrest (OHCA) survival rates.
83 per cent of all CFA brigades invited to participate in the program have accepted. As of 30 June 2025, 20 CFA brigades are operational and responding to Priority Zero events across rural and remote Victoria. A further 15 brigades are in training or preparing for training and consultation is continuing with remaining brigades.
Under this program, 33 per cent of all calls, where CFA are in attendance and resuscitation commenced, have achieved Return of Spontaneous Circulation (ROSC).
In partnership with the AV Registered Training Organisation, AV paramedics have so far provided nationally recognised training to over 350 CFA volunteers and provided 44 continuing education sessions across Victoria as part of the FMR program.
DH System Priority 4: A stronger workforce
There is increased supply of critical roles, which supports safe, high-quality care. Victoria is a world leader in employee experience, with a focus on future roles, capabilities and professional development.
The workforce is regenerative and sustainable, bringing a diversity of skills and experience that reflect the people and communities it serves.
As a result of a stronger workforce, Victorians receive the right care at the right time closer to home.
Goals
- Provide a safe, inclusive and well supported working environment where people feel valued, connected and empowered to effectively deliver the best patient-focused pre-hospital care.
- Continue to embed a culture of learning and improvement by building the capability of the workforce, including developing effective leadership.
- Explore new and contemporary models of care and practice, including future roles and capabilities.
AV Deliverables
1
AV will develop and implement a People Plan that sets out the goals, measures and approach for communication, engagement and recognition of employees and volunteers.
At the same time, AV will operationalise ‘AV Values’, to improve and evaluate the engagement, trust and job satisfaction of its people.
AV will have a particular focus on strategies and initiatives that help build morale and connection across all parts of AV, supporting a safe, fair and inclusive culture.
Associated Strategic Plan outcome
1.3 Our people are capable and continuously learn and grow
Associated AV Annual Plan Initiative
People Plan
AV Achievements
AV’s People Plan 2025-2028 was approved in June 2025. The People Plan describes key actions over the next three years to improve the experiences of our staff and volunteers.
These actions are aligned to the People pillar of the AV Strategic Plan 2023-2028 and reflect feedback from across the workforce about what is most important to them.
The People Plan focuses on supporting a diverse workforce, meaningful engagement, physical and psychological safety, capability development and leadership skills.
AV is continuing to operationalise our AV Values to strengthen engagement, trust, and improve morale and connection, by embedding them into AV documentation and programs (such the Upstander program), educating leaders and promoting values via various workshops and meetings.
2
Through the People Plan, AV will respond to the findings of the Victorian Equal Opportunity and Human Rights Commission (the Commission) Phase 3 evaluation audit and People Matter Survey results.
Associated Strategic Plan outcome
1.2 We are safe, healthy and well and we care for everyone
Associated AV Annual Plan Initiative
YourAV Program
AV Achievements
AV is continuing to respond to the Commission’s findings and has commenced an integrated response alongside the People Matters Survey results.
These ongoing actions now form part of the People Plan. AV continues to make progress in resetting expectations about appropriate workplace behaviours and creating a culture that is ‘values-driven’ and holds people to account for unlawful and harmful workplace conduct.
3
AV will develop and deliver a range of initiatives to improve workforce safety in 2024-25 including:
- improvements to staff mental health and wellbeing support and education
- implementation of a suicide prevention model
- implementation of a psychosocial risk framework to improve knowledge of psychosocial hazard exposure and management, and
- implementation of a prevention plan to address drivers of workplace harm developed in May 2024.
Associated Strategic Plan outcome
1.2 We are safe, healthy and well and we care for everyone
Associated AV Annual Plan Initiative
Mental Health and Wellbeing Action Plan
AV Achievements
AV continued to strengthen its commitment to mental health and wellbeing through a range of initiatives aligned with its Mental Health and Wellbeing Action Plan (MHWAP) 2022–2025 and broader organisational priorities addressing issues of stress and burnout.
AV developed and introduced a bespoke Suicide Intervention Response and Engagement Network (SIREN) learning package for suicide prevention.
AV’s psychosocial risk management approach details a hierarchy of controls for managing psychosocial hazards to prevent psychological harm to our people.
Preventing unlawful and harmful workplace behaviours is an ongoing responsibility of AV.
The Prevention Plan, now embedded in the People Plan, aims to support our people through increased safety, health, wellbeing, trust and morale; support the organisation by meeting legal obligations, attracting skilled workers and volunteers and increasing productivity; and support our patients through safer service delivery and improved experiences.
A range of activities across AV are focused on ensuring these prevention activities are a focal point of our work.
4
In partnership with its workforce, AV will implement changes related to the Ambulance Victoria Enterprise Agreement 2024.
Associated Strategic Plan outcome
1.2 We are safe, healthy and well and we care for everyone
Associated AV Annual Plan Initiative
Ambulance Victoria Enterprise Agreement 2024
AV Achievements
AV has implemented all increases to salaries, allowances, and continues to work through back payments.
AV is working with union partners on the implementation of all employee entitlements, including the significant additional end of shift protections for operational employees, which commence from 10 November 2025.
5
AV will continue to implement the actions defined in its Gender Equality Action Plan 2022-2025 (GEAP), ensuring AV makes meaningful and material progress towards organisational gender equality.
Associated Strategic Plan outcome
1.1 We are diverse. We are meaningfully engaged. We are valued.
Associated AV Annual Plan Initiative
Gender Equality Action Plan
AV Achievements
AV continues to make progress in gender equality aligned with the Gender Equality Act 2020 (Vic) and its GEAP.
AV has established a Gender Equality Working Group to oversee GEAP implementation, launched foundational resources (including learning modules, guides and policies), developed its first Gender Pay Gap Report (offering detailed, intersectional insights) participated in the Sponsorship of Diverse Talent Program with Emergency Management Victoria and improved inclusive recruitment tools and practices.
6
Lead cultural change in local teams to create a fair, safe and inclusive culture, AV will embed tools such as Upstander program and reflective practice and build the capability of frontline leaders through leadership training and a people leader toolkit.
Associated Strategic Plan outcome
1.2 We are safe, healthy and well and we care for everyone
Associated AV Annual Plan Initiative
YourAV Program
AV Achievements
In November 2024, AV commenced rolling out the Upstander program, educating and empowering our workforce to identify and respond to inappropriate behaviours and uphold our values.
AV also launched the Leading with Respect Program aimed at preventing and addressing sexual harassment and incivility.
In addition to these new initiatives, AV is continuing to run key leadership capability programs to build leadership performance and support cultural change. These include the Leading Together Program which builds the capability of our leaders; the Team Manager Toolkit that provides resources to support managers lead, Leading Wellbeing; Health Leaders, Healthy Teams.
DH System Priority 5: Moving from Competition to Collaboration
Share knowledge, information and resources with partner health and wellbeing services and care providers.
This will allow patients to experience one health, wellbeing and care system through connected digital health information, evidence, and data flows, enabled by advanced interoperable platforms.
Goals
- Form strategic partnerships with key stakeholders to provide high quality services and support improved health outcomes.
- Partner with consumers and their families to improve the design and delivery of ambulance services.
AV Deliverables
1
AV will implement a strategy for engaging with Triple Zero Victoria (TZV), to provide more efficient and effective progression of joint priorities, manage risks and escalate key issues.
Associated Strategic Plan outcome
4.2 External partnerships are efficient and effective
AV Achievements
AV and TZV work in close partnership to support our paramedics to deliver the best care to the Victorian community. AV and TZV continue to prioritise strengthening engagement and communication. This is critical to support strategic alignment, effective collaboration, strong governance and appropriate information sharing.
A new AV/TZV Initiatives Board has recently been established, to enhance collaboration, information sharing and to progress key shared priorities.
2
AV will continue to develop, deliver and lead authentic consumer engagement activities to improve the quality and accessibility of the services it provides. This will include building the capability of community engagement staff through the delivery of public engagement training and rollout of the AV consumer engagement playbook.
Associated Strategic Plan outcome
4.3 Our communities are resilient and informed
Associated AV Annual Plan Initiative
Community and Consumer Engagement Plan
AV Achievements
AV commenced delivery of the Regional Community Forums series, which provide an opportunity for Board, Executive and Community Advisory Committee members to connect with communities at a local level and directly hear the needs and views of ambulance users and communities.
AV also undertook extensive community engagement events and training.
The Co-design for Best Care (AV consumer engagement playbook) was released to AV staff in 2024. This guide helps staff to build confidence and capability in engaging and designing for, alongside and together with Victorian communities to create better services and models of care.
3
AV will foster an environment of continuous improvement and deliver demonstrable improvement in agreed key metrics through collaborative participation with stakeholders and sector partners. This is to be achieved, in part, through AV’s implementation of the Standards for Safe and Timely Ambulance and Emergency Care for Victorians, and AV TEC2.
Associated Strategic Plan outcome
2.3 Our clinical response model and provision of care is constantly evolving and sets best practice standards
Associated AV Annual Plan Initiative
Timely Emergency Care Program (TEC2)
AV Achievements
AV actively engages and collaborates with hospitals from across Victoria, Department of Health and other stakeholders to improve processes and services throughout the health care system.
In February 2025, new Standards for Safe and Timely Ambulance and Emergency Care for Victorians were released by the Minister for Health. AV has commenced embedding the standards into operational practice, including an update to operational work instructions to align with the new performance standards.
AV is continuing to progress the TEC2, which is a vehicle for implementing a consistent, robust approach to quality improvement. Through TEC 2 projects, AV is developing, testing, spreading, and scaling workforce-driven change ideas to improve patient care and create a safer, more satisfying workplace, initially in four focus areas; Daily Operating System, Transfer, Clearing, and Safe in Place (in field) which align with the new Standards.
4
AV will undertake community education and awareness programs, including Heart Safe Communities, Shocktober and Call Push Shock, to empower bystanders to provide CPR and use automated external defibrillators (AEDs) aiming to improving cardiac arrest survival.
Associated Strategic Plan outcome
4.3 Our communities are resilient and informed
Associated AV Annual Plan Initiative
Community and Consumer Engagement Plan
AV Achievements
AV continues to design and deliver engagement and education programs across metropolitan and regional Victoria to build community resilience and improve health outcomes for all Victorians.
In 2024-25, AV delivered 2,686 community engagement events reaching nearly 147,000 participants. This includes the following programs to improve cardiac arrest survival:
- Strong attendance at Heart Safe Communities and Call Push Shock sessions.
- A successful Shocktober program with significant community reach via face-to-face awareness sessions, social media, local media and online engagement tools.
- Facilitating CPR sessions and promoting the GoodSAM first responders program and public access AEDs.
5
AV will enhance processes and systems including decision support tools, performance monitoring and reporting, and staff and consumer engagement to increase safe utilisation of embedded alternate care pathways for older persons (RACER), frequent complex callers (patient coordination), and persons experiencing a mental health crisis (TelePROMPT/ TeleHELP).
Associated Strategic Plan outcome
2.1 All patients receive best care, improved health outcomes and experience
AV Achievements
In 2024-25, AV developed a triage service performance dashboard to support clearer visibility of alternate service provider utilisation and referrals. The dashboards have been successfully utilised for targeted education and to promote uptake of alternate service provider pathways by our teams to better service the community.
The introduction of the Complex Patient Escalation Pathway in conjunction with current workflows allow for escalation of care where required. This enables AV to identify and address the needs of this cohort to better meet their changing care goals.
Video triage for mental health nurses was introduced in September 2024 and work is continuing to embed this initiative and increase utilisation for improved assessments and outcomes. Ongoing education of infield staff has continued to increase utilisation of TelePROMPT service.
Performance priorities
Statement of Priorities Part B
High Quality & Safe Care
| 2024-25 Target | 2024-25 Actual | |
|---|---|---|
| Infection prevention and control | ||
| Percentage of healthcare workers immunised for influenza | 94% | 80% |
| Patient experience | ||
| Percentage of respondents who rated overall experience with the ambulance service as satisfied or very satisfied | 95% | 97% |
| Percentage of respondents who rated the level of care provided by paramedics as good or very good | 95% | 98% |
| Percentage of patients experiencing severe cardiac or traumatic pain whose level of pain was reduced significantly | 90% | 92.1% |
| Percentage of acute adult stroke patients transported to definitive care within 60 minutes | 90% | 97.8% |
| Percentage of major trauma patients that meet destination compliance (by 45 minutes) | 85% | 94.6% |
| Percentage of adult cardiac arrest patients surviving to hospital | 50% | 58.8% |
| Percentage of adult cardiac arrest patients surviving to hospital discharge | 25% | 38% |
Strong Governance, Leadership And Culture
| 2024-25 Target | 2024-25 Actual | |
|---|---|---|
| People Matter Survey – percentage of staff with an overall positive response to safety culture questions | 80% | 47% |
Timely Access to Care
| 2024-25 Target | 2024-25 Actual | |
|---|---|---|
| Percentage of emergency Code 1 incidents responded to within 15 minutes – statewide | 85% or improvement of 4 percentage points compared to the same time last year1 | 65.3% |
| Percentage of emergency Priority 0 incidents responded to within 13 minutes – statewide | 85% or improvement of 3 percentage points compared to the same time last year2 | 77.5% |
| Percentage of emergency Code 1 incidents responded to within 15 minutes in centres with a population greater than 7,500 | 90% or improvement of 3 percentage points compared to the same time last year3 | 69.2% |
| Percentage of triple zero cases where the caller receives advice or service from another health provider as an alternative to an emergency ambulance response – statewide | 20% or improvement of 3 percentage points compared to the same time last year4 | 19.5% |
| Percentage of patients transferred from ambulance to ED within 40 minutes | 90% or improvement of 4 percentage points compared to the same time last year5 | 68% |
| Average ambulance hospital clearing time | 20 mins | 31.4 mins |
- Last year’s result was 66.3% so 4 percentage point improvement would be 70.3%.
- Last year’s result was 77.3% so a 4 percentage point improvement would be 81.3%.
- Last year’s result was 70.2% so a 3 percentage point improvement would be 73.2%.
- Last year’s result was 17.1% so a 3 percentage point improvement would be 20.1%.
- Last year’s result was 65% so a 4 percentage point improvement would be 69%.
Effective financial management
| 2024-25 Target | 2024-25 Actual | |
|---|---|---|
| Operating Result ($m) | 0.0 | $54.9 |
| Adjusted Current Asset Ratio | 0.7 or 3% improvement from health service base target | 0.25 |
| Variance between forecast and actual Net Result from Transaction (NRFT) for the current financial year ending 30 June | 5% movement in forecast revenue and expenditure forecasts | 9.2% |
Relevant Ministers
Minister for Health
Minister for Ambulance Services
The Hon. Mary-Anne Thomas (1 July 2024 to 30 June 2025)
Statistical summary
Emergency Road Incidents2
Metropolitan Regions
| 2024-251 | 2023-241 | 2022-231 | 2021-22 | 2020-21 | 2019-20 | |
|---|---|---|---|---|---|---|
| Code 1 | 285,195 | 285,796 | 278,606 | 266,066 | 223,062 | 217,717 |
| Code 2 | 154,322 | 156,155 | 139,877 | 143,904 | 163,020 | 163,968 |
| Code 3 | 51,669 | 50,521 | 44,433 | 54,479 | 64,704 | 59,571 |
| Total Metropolitan Emergency Road Incidents | 491,186 | 492,472 | 462,916 | 464,449 | 450,786 | 441,256 |
Rural Regions3
| 2024-251 | 2023-241 | 2022-231 | 2021-22 | 2020-21 | 2019-20 | |
|---|---|---|---|---|---|---|
| Code 1 | 121,679 | 121,551 | 122,277 | 111,320 | 100,504 | 92,373 |
| Code 2 | 77,013 | 80,048 | 73,944 | 73,210 | 77,816 | 72,965 |
| Code 3 | 33,016 | 30,551 | 30,223 | 33,529 | 31,386 | 27,366 |
| Total Rural Emergency Road Incidents | 231,708 | 232,150 | 226,444 | 218,059 | 209,706 | 192,704 |
All Regions
| 2024-251 | 2023-241 | 2022-231 | 2021-22 | 2020-21 | 2019-20 | |
|---|---|---|---|---|---|---|
| Code 18 | 406,874 | 407,347 | 400,883 | 377,386 | 323,566 | 310,090 |
| Code 2 | 231,335 | 236,203 | 213,821 | 217,114 | 240,836 | 236,933 |
| Code 3 | 84,685 | 81,072 | 74,656 | 88,008 | 96,090 | 86,937 |
| Total Statewide Emergency Road Incidents | 722,894 | 724,622 | 689,360 | 682,508 | 660,492 | 633,960 |
Non-Emergency Road Incidents
| 2024-251 | 2023-241 | 2022-231 | 2021-22 | 2020-21 | 2019-20 | |
|---|---|---|---|---|---|---|
| Total Metropolitan Non-Emergency Road Incidents | 221,603 | 249,683 | 263,086 | 263,112 | 258,798 | 254,020 |
| Total Rural Non-Emergency Road Incidents | 83,896 | 110,771 | 100,835 | 97,282 | 96,748 | 85,710 |
| Total Statewide Non-Emergency Road Incidents | 305,499 | 360,454 | 363,921 | 360,394 | 355,546 | 339,730 |
| Total Metropolitan Road Incidents | 712,789 | 742,155 | 726,002 | 727,561 | 709,584 | 695,276 |
| Total Rural Road Incidents | 315,604 | 342,921 | 327,279 | 315,341 | 306,454 | 278,414 |
Road Incidents
All Regions
| 2024-251 | 2023-241 | 2022-231 | 2021-22 | 2020-21 | 2019-20 | |
|---|---|---|---|---|---|---|
| Emergency Code 1 | 406,874 | 407,347 | 400,883 | 377,386 | 323,566 | 310,090 |
| Emergency Code 2 | 231,335 | 236,203 | 213,821 | 217,114 | 240,836 | 236,933 |
| Emergency Code 3 | 84,685 | 81,072 | 74,656 | 88,008 | 96,090 | 86,937 |
| Non-Emergency | 305,499 | 360,454 | 363,921 | 360,394 | 355,546 | 339,730 |
| Total Road Incidents | 1,028,393 | 1,085,076 | 1,053,281 | 1,042,902 | 1,016,038 | 973,690 |
Air Incidents
All Regions
| 2024-251 | 2023-241 | 2022-231 | 2021-22 | 2020-21 | 2019-20 | |
|---|---|---|---|---|---|---|
| Fixed Wing – Emergency | 1,982 | 2,045 | 2,179 | 1,962 | 2,017 | 1,771 |
| Fixed Wing – Non-Emergency | 2,818 | 3,310 | 3,288 | 3,320 | 3,048 | 2,693 |
| Total Fixed Wing Incidents | 4,800 | 5,355 | 5,467 | 5,282 | 5,065 | 4,464 |
| Helicopter Incidents (All Emergency) | 2,216 | 2,387 | 2,422 | 2,476 | 2,642 | 2,343 |
| Emergency Air Incidents | 4,198 | 4,432 | 4,601 | 4,438 | 4,659 | 4,114 |
| Non-Emergency Air Incidents | 2,818 | 3,310 | 3,288 | 3,320 | 3,048 | 2,693 |
| Total Air Incidents | 7,016 | 7,742 | 7,889 | 7,758 | 7,707 | 6,807 |
Adult Retrieval
| 2024-251 | 2023-241 | 2022-231 | 2021-22 | 2020-21 | 2019-20 | |
|---|---|---|---|---|---|---|
| Cases handled | 7,131 | 7,110 | 6,562 | 6,365 | 5,587 | 4,833 |
Retrievals
| 2024-251 | 2023-241 | 2022-231 | 2021-22 | 2020-21 | 2019-20 | |
|---|---|---|---|---|---|---|
| Road retrievals – ARV Crew (Doctors and/or Critical Care Registered Nurse) | 520 | 540 | 651 | 829 | 571 | 474 |
| Road retrievals – paramedic only | 808 | 770 | 575 | 456 | 477 | 424 |
| Road retrievals – doctor & paramedic | 237 | 202 | 195 | 218 | 218 | 183 |
| Total road retrievals | 1,565 | 1,512 | 1,421 | 1,503 | 1,266 | 1,081 |
| Air retrievals – paramedic only | 1,175 | 1,349 | 1,319 | 1,217 | 1,161 | 1,023 |
| Air retrievals – doctor & paramedic | 512 | 471 | 478 | 376 | 531 | 476 |
| Total air retrievals | 1,687 | 1,820 | 1,797 | 1,593 | 1,692 | 1,499 |
| Total adult retrievals | 3,252 | 3,332 | 3,218 | 3,096 | 2,958 | 2,580 |
Code 1 Response Time
| 2024-251 | 2023-241 | 2022-231 | 2021-22 | 2020-21 | 2019-20 | |
|---|---|---|---|---|---|---|
| Proportion of emergency (Code 1) incidents responded to in 15 minutes or less | 65.3% | 66.3% | 62.8% | 67.5% | 77.2% | 82.3% |
| Proportion of emergency (Code 1) incidents, located in centres with a population greater than 7,500, and responded to in 15 minutes or less4 | 69.2% | 70.2% | 66.5% | 71.9% | 82.5% | 87.6% |
Referral Service
| 2024-251 | 2023-241 | 2022-231 | 2021-22 | 2020-21 | 2019-20 | |
|---|---|---|---|---|---|---|
| Percentage of 000 cases resulting in callers receiving health advice or service from another health provider as an alternative to emergency ambulance response5 | 19.5% | 17.7% | 18.7% | 19.8% | 17.6% | 17.6% |
Patients Transported2
Road transports (Metropolitan Regions)
| 2024-251 | 2023-241 | 2022-231 | 2021-22 | 2020-21 | 2019-20 | |
|---|---|---|---|---|---|---|
| Emergency Operations | 320,023 | 330,771 | 327,431 | 336,652 | 349,714 | 342,400 |
| Non-Emergency Operations Stretcher | 123,651 | 131,966 | 140,764 | 146,139 | 141,464 | 137,461 |
| Non-Emergency Clinic Transport Services | 79,582 | 101,245 | 96,709 | 93,025 | 99,104 | 100,234 |
| Total Metropolitan Regions | 523,256 | 563,982 | 564,904 | 575,816 | 590,282 | 580,095 |
Road Transports (Rural Regions)3
| 2024-251 | 2023-241 | 2022-231 | 2021-22 | 2020-21 | 2019-20 | |
|---|---|---|---|---|---|---|
| Emergency Operations | 164,853 | 171,351 | 168,889 | 167,167 | 168,930 | 156,326 |
| Non-Emergency Operations Stretcher | 54,280 | 58,529 | 60,273 | 62,177 | 67,670 | 68,507 |
| Total Rural Regions3 | 219,133 | 229,880 | 229,162 | 229,344 | 236,600 | 224,833 |
| Total Patients Transported by Road | 742,389 | 793,862 | 794,066 | 805,160 | 826,882 | 804,928 |
Air Transports (All Regions)
| 2024-251 | 2023-241 | 2022-231 | 2021-22 | 2020-21 | 2019-20 | |
|---|---|---|---|---|---|---|
| Fixed Wing transports | 3,933 | 4,445 | 5,062 | 4,835 | 4,699 | 4,333 |
| Total Helicopter Transports | 1,818 | 1,963 | 1,950 | 1,981 | 2,159 | 1,973 |
| Total Air Transports | 5,751 | 6,408 | 7,012 | 6,816 | 6,858 | 6,306 |
| 2024-251 | 2023-241 | 2022-231 | 2021-22 | 2020-21 | 2019-20 | |
|---|---|---|---|---|---|---|
| Total Patient Transports | 748,140 | 800,270 | 801,078 | 811,338 | 833,740 | 811,234 |
Road Patients Transported (All Regions) – Charging Categories6
Compensable Transports
| 2024-251 | 2023-241 | 2022-231 | 2021-22 | 2020-21 | 2019-20 | |
|---|---|---|---|---|---|---|
| Veterans' Affairs | NA | 9,548 | 10,552 | 12,605 | 14,199 | 16,400 |
| Transport Accident Commission | NA | 13,668 | 13,853 | 12,804 | 13,055 | 14,701 |
| WorkCover | NA | 3,044 | 3,055 | 3,207 | 3,778 | 3,697 |
| Public Hospital Transfers | NA | 35,892 | 35,767 | 32,032 | 30,306 | 27,949 |
| Private Hospital Transfers | NA | 2,193 | 2,576 | 2,541 | 2,389 | 2,226 |
| Ordinary | NA | 69,312 | 69,824 | 67,363 | 62,315 | 62,790 |
| Subscriber | NA | 155,403 | 159,389 | 165,995 | 164,165 | 155,817 |
| Total Compensable Road Transports | NA | 289,060 | 295,016 | 296,547 | 290,207 | 283,580 |
| Community Service Obligation Road Transports | NA | 486,032 | 489,062 | 500,833 | 528,933 | 513,545 |
| Other7 | NA | 18,770 | 9,988 | 7,780 | 7,742 | 7,803 |
| Total Patients Transported by Road | 742,389 | 793,862 | 794,066 | 805,160 | 826,882 | 804,928 |
Notes
1. Figures for 2023-24 have been updated where applicable to include data received after the completion of last year’s report. Figures for 2024-25 are subject to change, and will be updated accordingly.
2. Prior to 2023-24, incidents and transports were categorised as metropolitan or rural based on the location of the resource used. This has been updated to location of the incident to more accurately reflect demand, and avoid double counting. The impact to reported figures is <0.5%, and data is comparable to previous years.
3. Rural regions includes cross-border responses into NSW and SA.
4. Based on the Australian Bureau of Statistics Urban Centre boundaries and resident population data.
5. Referral results have been updated to include doctor request (CLINMRT) and referral welfare check cases that were diverted from emergency dispatch. This change has been implemented to correct an inconsistency between Emergency and Referral Services reporting. Figures prior to 2019/2020 are incomparable.
6. The charge class assigned to patients transported is subject to change during the period when an account is being finalised, and significant movements between charge classes can occur after the end of the financial year. Charge class figures for 2024-25 are “NA” due to delays in accessing this data during protected industrial action
7. The “other” category includes the road components of multi-legged road transports which have not been assigned a charge class. The “Other” category also includes road transports not yet assigned a charge class.
8. Refers to the total Code 1 statewide emergency road incidents. This figure includes both attended and not attended. Reasons for non-attendance to Code 1 cases includes duplicate calls, unable to locate, cancellations by the caller or other emergency service, and referrals to alternate pathways.
Statutory compliance
Freedom of Information Act 1982
Ambulance Victoria (AV) received 2,991 requests (three of these requests were transferred to AV from other agencies) under the Freedom of Information Act 1982 (the Act) for the 2024-25 FY.
Full access to documents was provided in 1,793 requests.
Exemptions under the Act were applied to 637 requests.
Partial access was granted for 637 requests whilst three requests were denied in full.
The most common reason for AV seeking to partially exempt documents was the protection of personal privacy in relation to request for information about persons other than the applicant. Other exemptions applied under the Act included internal working documents, documents containing material obtained in confidence and documents relating to trade secrets, etc.
The below table shows most applications were received from members of the public, doctors/hospitals and solicitors. The Freedom of Information (FOI) unit also received requests from media and Members of Parliament.
Non-statute FOI requests 2024-25
| Origin of request | Requests |
|---|---|
| Public | 436 |
| Dr/Hospital | 497 |
| Insurance | 178 |
| Media | 2 |
| Member of Parliament | 4 |
| Solicitor | 1,797 |
| Other | 37 |
| Psychologist | 22 |
| WorkCover | 18 |
| Total | 2,991 |
The FOI unit collected $66,960.80 in application fees under The Act. AV collected nil dollars in access charge fees to facilitate access to documents. In addition, the FOI unit processed the below requests outside of the Act applying the relevant statute law.
Statute FOI requests 2024-25
| Origin of request | Requests |
|---|---|
| Coroner | 374 |
| Child Protection/DFFH | 270 |
| TAC | 542 |
| Aged Care Commissioner | 6 |
| Other | 34 |
| Medical Practitioners Board | - |
| Total | 1,226 |
| FOI requests | 2024-25 |
|---|---|
| Requests received during the year | 2,988* |
| Request transferred to another agency | 0 |
| Request transferred from another agency | 3 |
| Request withdrawn or not proceed with by the applicant | 91 |
| Access granted in full | 1,793 |
| Access granted in part (exemptions applied) | 637 |
| Access denied in full (exemptions applied) | 3 |
| Request where no relevant documents could be located | 264 |
| Request not deemed valid | 102 |
| Requests awaiting completion at the end of the FY | 101 |
| Request not completed within the statutory period of 30 days | 153 |
*Total requests was 2,991, with three of these requests transferred to AV from other agencies.
| Office of the Victorian Information Commissioner and VCAT 2024-25 | |
|---|---|
| Reviews/Complaints accepted by FOI Commissioner | 5 |
| VCAT appeal lodged | 1 |
Victoria Police
The FOI unit also processed the following requests from Victoria Police for patient care records and paramedic statements and processed subpoenas for documents and summons for documents and paramedics to attend court.
| Victoria Police requests | |
|---|---|
| PCR only | 737 |
| Statement only | 384 |
| PCR and statements | 361 |
| PCR, statements & details | 6 |
| Statements & details | 28 |
| PCR and details | 28 |
| Paramedic details | 106 |
| Other request | 103 |
| Total | 1,753 |
| Subpoena/Summons | |
|---|---|
| To attend court | 61 |
| To produce documents | 137 |
| Total | 198 |
Carers Recognition Act 2012
AV acknowledges the essential contribution carers make to the wellbeing of individuals and the broader community. In alignment with statutory obligations and our organisational values, AV remains committed to ensuring that our services and workforce practices uphold the rights and needs of carers. We continue to embed carer recognition across our operations and strengthen practices that support carers both as service users and employees.
Building Act 1993
AV is compliant with Victoria’s legislative framework for building activity. All building construction during the year was conducted in accordance with the requirements of the Building Act 1993, the Building Regulations 2018 and the applicable provisions of the National Construction Code. These frameworks collectively govern the design, construction, and maintenance of new ambulance stations, refurbishment of existing facilities or when undertaking building fit outs.
Maintenance and annual reporting of Essential Safety Measures (ESM) form a critical component of Ambulance Victoria’s governance and compliance obligations. All ESM reporting and maintenance was completed in accordance with requirements of the Building Regulations 2018.
Public Interest Disclosures Act 2012
Under the Public Interest Disclosures Act 2012, complaints and allegations about improper conduct involving public health services in Victoria should be made directly to the Independent Broad-based Anti-Corruption Commission (IBAC). AV is required to encourage concerned individuals to make relevant public interest disclosures (within the meaning of the Act) directly to IBAC and to establish and publish public interest disclosures policy and procedures.
Statement on National Competition Policy
The State of Victoria is a party to the intergovernmental Competition Principles Agreement, which is a key document in Australia’s National Competition Policy framework. The Victorian Government is committed to the ongoing implementation of the National Competition Policy in a considered and responsible manner.
This means public interest considerations should be taken into account explicitly in any government decisions on the implementation of this policy. AV adheres to this and complies, to the extent applicable, with the National Competition Policy.
Gender Equality Act 2020
As a defined entity under the Gender Equality Act 2020, AV has been progressively taking steps to meet its legislative obligations. This year we continued our implementation of the Gender Equality Action Plan 2022-2025 including establishment of a cross-functional gender equality working group, development of the inclusive language guide, active engagement across the health, emergency services and government sector, continued to investigate the impacts of the gender pay gap, and developed an approach for the collection of diversity data.
AV continues to report to the Commission for Gender Equality in the Public Sector on our progress, including a Workplace Gender Audit.
Local Jobs First Act 2003
The Local Jobs First Act 2003 applies to all projects valued at $3 million or more in metropolitan Melbourne or state-wide. The policy also applies to projects in regional Victoria valued at $1 million or more.
During 2024-25 AV commenced three Local Jobs First Standard contracts totalling $38.6 million. All contracts were state-wide.
The Local Jobs First commitment outcomes expected from these contracts are:
- An average of 91.51 per cent of local content committed.
- A total of 168.44 jobs (annualised employee equivalent) committed, including the creation of 63.72 new jobs and the retention of 104.72 jobs.
- A total of 19.28 positions for apprentices, trainees and cadets committed, including the creation of 18.61 new apprenticeships, traineeships and cadets, and the retention of 0.67 existing apprenticeships, traineeships and cadets.
During 2024-25 AV completed four contracts subject to the Local Jobs First policy totalling $276.86 million. Three of these contracts were statewide. The Major Project Skills Guarantee Policy applies to all construction projects valued at $20 million or more. No projects during 2024-25 were subject to policy.
Code of Conduct
AV employees are subject to the Code of Conduct for Victorian Public Sector Employees (Code). AV has policies and procedures that are consistent with the Code. These documents contain the expected workplace conduct and behaviours specific to AV.
The AV Code of Conduct is built on our values, professional and ethical standards, and the additional obligations we are required to adhere to as a Victorian Government Agency. Our policies and procedures are reviewed on a regular basis to ensure compliance with our legal obligations.
Additional information available upon request
In compliance with the Standing Directions 2018 under the Financial Management Act 1994, AV advises that the following information, where applicable, is available to the Minister for Ambulance Services, Members of Parliament, and the public on request (subject to the provisions of the Freedom of Information Act 1982):
Declarations of pecuniary interests have been duly completed by all relevant officers.
- Details of shares held by senior officers as nominee or held beneficially.
- Details of publications produced by the entity about AV, and how these can be obtained.
- Details of changes in prices, fees, charges, rates and levies charged by AV.
- Details of any major external reviews carried out on AV.
- Details of major research and development activities undertaken by AV that are not otherwise covered either in the report of operations or in a document that contains the financial statements and report of operations.
- Details of overseas visits undertaken including a summary of the objectives and outcomes of each visit.
- Details of major promotional, public relations and marketing activities undertaken by AV to develop community awareness of AV and its services.
- Details of assessments and measures undertaken to improve the occupational health and safety of employees.
- A general statement on industrial relations within AV and details of time lost through industrial accidents and disputes, which is not otherwise detailed in the report of operations.
- A list of major committees sponsored by AV, the purposes of each committee and the extent to which those purposes have been achieved.
Details of all consultancies and contractors including consultants/contractors engaged, services provided, and expenditure committed for each engagement. The AV website contains information about AV and is regularly updated with the latest statistics, developments and media releases.
Requests for access to this information can be directed to AV’s FOI unit.
Consultancies
Details of consultancies (under $10,000)
In 2024-25, there was one consultancy where the total fees payable to the consultants were less than $10,000. The total expenditure incurred during 2024-25 in relation to these consultancies was $1,382 (excluding GST).
Details of consultancies (valued at $10,000 or greater)
In 2024-25, there were four consultancies where the total fees payable to the consultants were $10,000 or greater. The total expenditure incurred during 2024-25 in relation to these consultancies was $217,250 (excluding GST). Details of individual consultancies are below.
Details of individual consultancies – over $10,000
| Consultant Name | Purpose of Consultancy | Start date | End date | Total Approved Project Fee (excl GST) $’000 | Expenditure 2024-25 $’000 | Future Expenditure (excl GST) $’000 |
|---|---|---|---|---|---|---|
| Macutex Pty Ltd | Building Condition and Function Audit | Oct 2023 | Oct 2027 | 971 | 84 | 515 |
| Mayfield Advisory Pty Ltd | Independent Financial Support and Advice | Mar 2025 | Jun 2025 | 69 | 76* | 30** |
| Workwell Consulting Pty Ltd | Board Reflective Practice Workshop | Nov 2024 | Nov 2024 | 15 | 15 | – |
| Perfekt Pty Ltd | Data Backup and Recovery recommendations provided for Cloud Migration project | Jun 2023 | Oct 2024 | 13 | 13 | – |
*Expenditure exceeded approved project fee due to additional work undertaken.
**Expected expenditure pending approval.
Government advertising campaign
Nil reports.
ICT expenditure
For the 2024-25 reporting period, AV had a total ICT expenditure of $43.38m (excl. GST) with the details shown below ($m).
| All operational ICT Expenditure | ICT Expenditure related to projects to create or enhance ICT capabilities | |
|---|---|---|
| Business As Usual (BAU) ICT expenditure (Total) | Non Business As Usual (non BAU) ICT expenditure (Total = Operating expenditure and Capital Expenditure) | |
| $41.33m | $2.05m | |
| Operating Expenditure | Capital Expenditure | |
| $2.04m | $0.01m | |
Financial summary
AV achieved a $27.5m net result surplus for 2024-25.
A 10.5 per cent increase in 2024-25 income contributed to the surplus, which was largely driven by additional government funding to support the implementation of the new enterprise agreement and ongoing operational needs.
The increased revenue also reflected a partial recovery of transport fee income from the prior year, which had been adversely impacted by Protected Industrial Action, commencing in March 2024, limiting AV’s ability to invoice patients. During 2024-25, AV prioritised efforts to retrospectively bill for eligible services from the prior year, ensuring lost income was recovered where possible.
Expenditure increased 6.6 per cent, which was predominately influenced by higher salary costs resulting from the implementation of the new enterprise agreement.
Higher expenditure was also experienced due to increased demand, new contracts related to Air Ambulance and Non-Emergency Transport delivery services, and the commencement of the rollout of iPads to all paramedics.
| Summary of Financial Results | 2024-25 $000 | 2023-24 $000 | 2022-23 $000 | 2021-22 $000 | 2020-21 $000 |
|---|---|---|---|---|---|
| Total Income from Transactions | 1,638,311 | 1,482,636 | 1,614,373 | 1,481,874 | 1,288,269 |
| Total Expenses from Transactions | (1,593,283) | (1,494,416) | (1,607,483) | (1,453,587) | (1,298,929) |
| Net Result from Transactions | 45,028 | (11,780) | 6,890 | 28,287 | (10,660) |
| Total Other Economic Flows | (17,566) | (14,940) | (44,133) | 357 | 10,891 |
| Net Result | 27,462 | (26,720) | (37,243) | 28,644 | 231 |
| Total Assets | 1,386,607 | 1,399,989 | 1,039,734 | 1,065,675 | 1,051,955 |
| Total Liabilities | 938,576 | 960,655 | 702,954 | 716,849 | 749,793 |
| Net Assets | 448,031 | 439,333 | 336,780 | 348,826 | 302,162 |
| Reconciliation between Net Result from Transactions AND Statement of Priorities | 2024-25 $000 |
|---|---|
| SOP Operating Result | 54,895 |
| Capital and Specific Items | |
| Capital Purpose Income | 125,532 |
| Specific Income | – |
| Assets Received Free of Charge | 2 |
| Assets Provided Free of Charge | – |
| Other Non-Operating Expenses | (153) |
| Depreciation and Amortisation | (113,607) |
| Impairment of Non-Financial Assets | – |
| Finance Costs | (21,641) |
| Net Result from Transactions | 45,028 |
Asset management accountability framework
Asset Management Accountability Framework (AMAF) maturity self-assessment
The following section summarises AV’s self-assessment of maturity against the requirements of the Asset Management Accountability Framework (AMAF). The AMAF is a non-prescriptive, devolved accountability model of asset management that requires compliance with 41 mandatory requirements. These requirements can be found on the DTF website at www.dtf.vic.gov.au/asset-management-accountability-framework.
AV’s target maturity rating is ‘competence’, meaning systems and processes are fully in place, consistently applied and systematically meeting the AMAF requirements, including a continuous improvement process to expand system performance above AMAF minimum requirements.
Results
Leadership and accountability (requirements 1-19)
AV has met its target maturity level for most of the requirements within this category. AV is partially compliant with some requirements relating to asset assessment and monitoring. There were no material non-compliances reported in this category.
There are initiatives and plans for improvement currently underway to improve AV’s maturity rating in these areas. These include completion of an organisation-wide assessment of asset criticality and improvements to the asset performance reporting process.
Planning (requirements 20-23)
AV has met its target maturity level in this category.
Acquisition (requirements 24 and 25)
AV has met its target maturity level in this category.
Operation (requirements 26-40)
AV has met its target maturity level for some requirements within this category, and is working toward compliance in the areas of monitoring and preventative action, maintenance systems and processes, reporting, and information management. There were no material non-compliances reported in this category.
AV is developing a plan to aggregate and modernise the capture of asset information with improved functionality for planning, monitoring and reporting of asset performance to enhance the organisation’s ability to proactively identify potential asset performance failures and identify options for preventive action. This will also further mature the organisation’s information management and record keeping practices.
Disposal (requirement 41)
AV has met its target maturity level in this category.
| AMAF Maturity Level | Scale |
|---|---|
| Innocence | 0 |
| Awareness | 1 |
| Developing | 2 |
| Competence | 3 |
| Optimising | 4 |
Disclosure index
The annual report of Ambulance Victoria is prepared in accordance with all relevant Victorian legislation. This index has been prepared to facilitate identification of the department’s compliance with statutory disclosure requirements.
Report of operations
Charter and purpose
| Legislation | Requirement | Page |
|---|---|---|
| FRD 22 | Manner of establishment and the relevant Ministers | 58, 83 |
| FRD 22 | Purpose, functions, powers, and duties | 8-61 |
| FRD 22 | Nature and range of services provided | 8-61 |
| FRD 22 | Activities, programs, and achievements for the reporting period | 8-61 |
| FRD 22 | Significant changes in key initiatives and expectations for the future | 8-61 |
Management and structure
| Legislation | Requirement | Page |
|---|---|---|
| FRD 22 | Organisational structure | 69 |
| FRD 22 | Workforce data/employment and conduct principles | 42 |
| FRD 22 | Workforce inclusion policy | 88-91 |
| FRD 22 | Occupational Health and Safety | 43-44 |
Financial and other information
| Legislation | Requirement | Page |
|---|---|---|
| FRD 22 | Summary of the financial results for the year | 94 |
| FRD 22 | Significant changes in financial position during the year | 94 |
| FRD 22 | Operational and budgetary objectives and performance against objectives | 70-81, 84-87 |
| FRD 22 | Subsequent events | 129 |
| FRD 22 | Details of consultancies under $10,000 | 92 |
| FRD 22 | Details of consultancies over $10,000 | 92 |
| FRD 22 | Disclosure of government advertising expenditure | Nil to report |
| FRD 22 | Disclosure of ICT expenditure | 93 |
| FRD 22 | Asset Management Accountability Framework | 95 |
| FRD 22 | Disclosure of emergency procurement | Nil to report |
| FRD 22 | Disclosure of social procurement activities under the Social Procurement Framework | 53 |
| FRD 22 | Disclosure of procurement complaints | Nil to report |
| FRD 22 | Disclosure of reviews and study expenses | Nil to report |
| FRD 22 | Disclosure of grants and transfer payments | Nil to report |
| FRD 22 | Application and operation of Freedom of Information Act 1982 | 88 |
| FRD 22 | Compliance with building and maintenance provisions of Building Act 1993 | 89 |
| FRD 22 | Application and operation of Public Interest Disclosure Act 2012 | 90 |
| FRD 22 | Statement on National Competition Policy | 90 |
| FRD 22 | Application and operation of Carers Recognition Act 2012 | 89 |
| FRD 22 | Additional information available on request | 91 |
| FRD 24 | Environmental data reporting | 45 |
| FRD 25 | Local Jobs First Act 2003 disclosures | 90 |
Compliance attestation and declaration
| Legislation | Requirement | Page |
|---|---|---|
| SD 5.1.4 | Financial Management Compliance attestation | 11 |
| SD 5.2.3 | Declaration in Report of Operations | 11-13 |
| Attestation on Data Integrity | 12 | |
| Attestation on managing Conflicts of Interest | 13 | |
| Attestation on Integrity, Fraud, and Corruption | 12 | |
| Compliance with Health Share Victoria (HSV) Purchasing Policies | 13 |
Other reporting requirements
| Legislation | Requirement | Page |
|---|---|---|
| Reporting of outcomes from Statement of Priorities 2024-2025 | 70-83 | |
| Occupational Violence reporting | 44 |
Financial statements
Declaration
| Legislation | Requirement | Page |
|---|---|---|
| SD 5.2.2 | Declaration in financial statements | 98-100 |
Other requirements under Standing Directions 5.2
| Legislation | Requirement | Page |
|---|---|---|
| SD 5.2.1(a) | Compliance with Australian accounting standards and other authoritative pronouncements | Note 1.1 |
| SD 5.2.1(a) | Compliance with Standing Directions | Per declaration p1 |
Other disclosures as required by FRDs in notes to the financial statements
| Legislation | Requirement | Page |
|---|---|---|
| FRD 11 | Disclosure of Ex gratia Expenses | Note 8.6 |
| FRD 103 | Non-Financial Physical Assets | Note 4.1 |
| FRD 110 | Cash Flow Statements | Note 8.1 |
| FRD 112 | Defined Benefit Superannuation Obligations | Note 3.1(c) |
| FRD 114 | Financial Instruments – general government entities and public non-financial corporations | Note 7.1 |
Financial report
Board Chair’s, Chief Executive Officer’s and Chief Financial Officer’s Declaration
The attached financial statements for Ambulance Victoria have been prepared in accordance with Direction 5.2 of the Standing Directions of the Minister for Finance under the Financial Management Act 1994, applicable Financial Reporting Directions, Australian Accounting Standards including Interpretations, and other mandatory professional reporting requirements.
We further state that, in our opinion, the information set out in the comprehensive operating statement, balance sheet, statement of changes in equity, cash flow statement and accompanying notes, presents fairly the financial transactions during the year ended 30 June 2025 and the financial position of Ambulance Victoria at 30 June 2025.
At the time of signing, we are not aware of any circumstance which would render any particulars included in the financial statements to be misleading or inaccurate.
We authorise the attached financial statements for issue on 6 October 2025.
Andrew Crisp
Board Chair
Melbourne
6 October 2025
Jordan Emery
Chief Executive Officer
Melbourne
6 October 2025
Jessica Lambous
Chief Financial Officer
Melbourne
6 October 2025